An inlet patch (IP) is the presence of gastric columnar epithelium outside of the stomach. No studies have been conducted in Mexico on that pathology. The aim of the present study was to determine the prevalence of esophageal IP and the clinical characteristics of the patients that present it.
Materials and methodsA cross-sectional study was conducted that included consecutive patients referred for endoscopy within the time frame of September 2015 to May 2016. The patients answered a questionnaire, and high-definition endoscopy with digital chromoendoscopy was performed. The prevalence of IP was identified. The chi-square test was used to compare the clinical characteristics between patients that presented with esophageal IP and those without it.
ResultsA total of 239 patients were included in the study. Their mean age was 53 years, and 130 (54.4%) were women. IP was found in 26 patients (10.9%), 15 of whom were men (57.7%). The main reason for referral to endoscopy was gastroesophageal reflux disease, present in 69.2% of the patients with IP and in 55.9% without IP (p=.19). The most common symptoms were heartburn and regurgitation. The former was present in 69.2% of the patients with IP and in 59.1% without IP (p=.32), and the latter was present in 65.4% of the patients with IP and 69.1% without IP (p=.7). Extraesophageal manifestation distribution was: cough in 46.2% of the patients with IP and 38% without IP (p=.45) and dysphonia in 54% with IP and 47% without IP (p=.53). Twenty-three percent of the patients with IP had Barrett's esophagus, as did 23% without IP (p=.99).
ConclusionsThe prevalence of IP was high. The primary referral diagnosis was gastroesophageal reflux disease. No differences were found in relation to symptoms or the presence of Barrett's esophagus between the patients with and without IP.
El parche de mucosa gástrica ectópica (inlet patch [IP]) es la presencia de mucosa columnar gástrica fuera del estómago. En nuestro país no se ha realizado ningún estudio sobre esta patología. El objetivo es determinar la prevalencia y características clínicas de pacientes que presentan IP en el esófago.
Material y métodosEstudio transversal. Se incluyeron pacientes consecutivos enviados a endoscopía de septiembre de 2015 a mayo de 2016. Se les aplicó un cuestionario de manifestaciones clínicas y se realizó endoscopía con equipo de alta definición y cromoendoscopía digital. Se identificó la prevalencia de IP. Se contrastaron las características clínicas del grupo afectado con el resto del grupo mediante chi cuadrada.
ResultadosSe incluyeron 239 pacientes, edad promedio 53 años, 130 (54.4%) mujeres. Se encontró IP en 26 pacientes (10.9%), 15 hombres (57.7%). El principal motivo de envío fue enfermedad por reflujo gastroesofágico en 69.2% de los pacientes con IP y 55.9% sin IP (p=0.19). Los principales síntomas fueron pirosis: 69.2% con IP, 59.1% sin IP (p=0.32) y regurgitaciones 65.4% con IP, 69.1% sin IP (p=0.7). La distribución de las manifestaciones extraesofágicas fueron: tos 46.2% con IP, 38% sin IP (p=0.45) y disfonía 54% con IP, 47% sin IP (p=0.53). Presencia de esófago de Barrett en 23.0% de pacientes con IP y 23% sin IP (p=0.99).
ConclusionesLa prevalencia de IP fue alta. El principal diagnóstico de envío fue enfermedad por reflujo gastroesofágico. No se encontraron diferencias en síntomas ni en presencia de esófago de Barrett en pacientes con y sin IP.
The inlet patch (IP) is the presence of gastric columnar epithelium outside of the stomach. It was first described in 1805 by Schmidt,1 and incidence ranges from 1 to 13.8%. Although widely considered congenital, there are 3 theories on its origin: acquired metaplastic transformation, congenital origin, and rupture of glandular cysts.2 It can present in the entire digestive tract, from the tongue to the rectum, or in extraluminal sites such as the gallbladder, cystic duct, omphalomesenteric duct, umbilicus, and liver.2 However, the most frequent location is the cervical esophagus, mainly in the 3cm below the upper esophageal sphincter. When it presents in the distal esophagus, it must be differentiated from Barrett's esophagus.3
The most common epithelium is the cardia with oxyntic cells, followed by the antral mucosa. Some IPs can produce acid.4 They are generally asymptomatic and only detected incidentally at upper endoscopy. IP is associated with gastroesophageal reflux disease (GERD), and esophageal and extraesophageal syndromes.5,6 It is also associated with complications such as dysphagia, stricture, ulcers, tracheoesophageal fistula, acute esophageal perforation, polyps, membranes, bleeding, premalignant conditions, carcinomas,1,7,8 and with the presence of Helicobacter pylori (H. pylori) at that site.8–10
The aim of the present study was to determine the prevalence of IP and its association with clinical characteristics through directed search using digital chromoendoscopy in patients undergoing endoscopy.
Materials and methodsA descriptive, cross-sectional study was conducted at an outpatient endoscopy unit in the city of Puebla, within the time frame of September 2015 to May 2016. It included consecutively selected older patients referred for upper endoscopy that agreed to participate in the study. The patients that met the inclusion criteria were examined by a single endoscopist. Patients with psychiatric illness, severe systemic disease, or undergoing endoscopy for bleeding were excluded from the study. The eliminated patients were those that asked to be removed from the study.
Before the endoscopic procedure, the patients answered a questionnaire to provide their sociodemographic data, as well as the amount of time they had with GERD symptoms (heartburn, regurgitation, cough, dysphonia, globus sensation, and dysphagia).
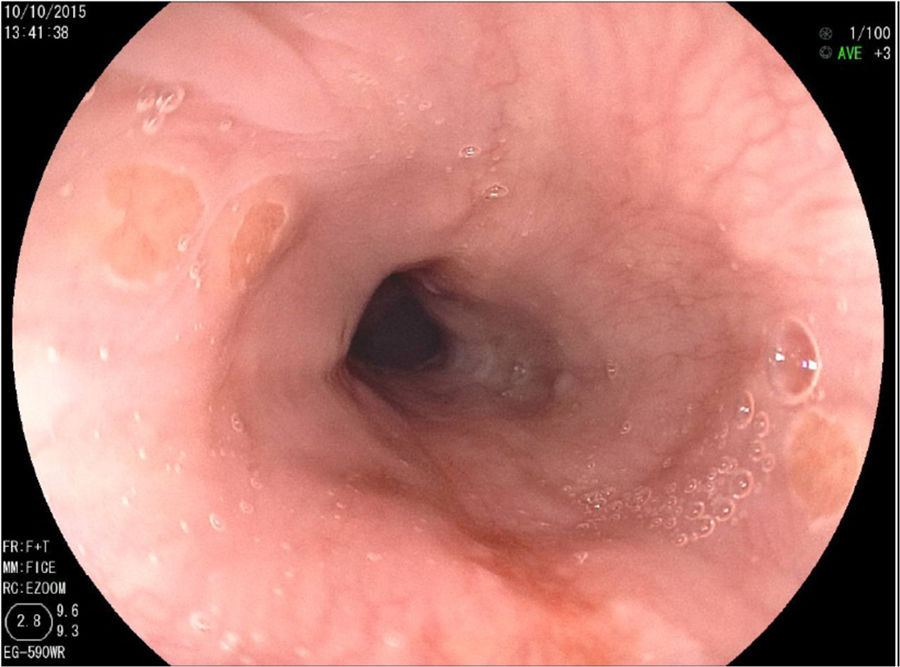
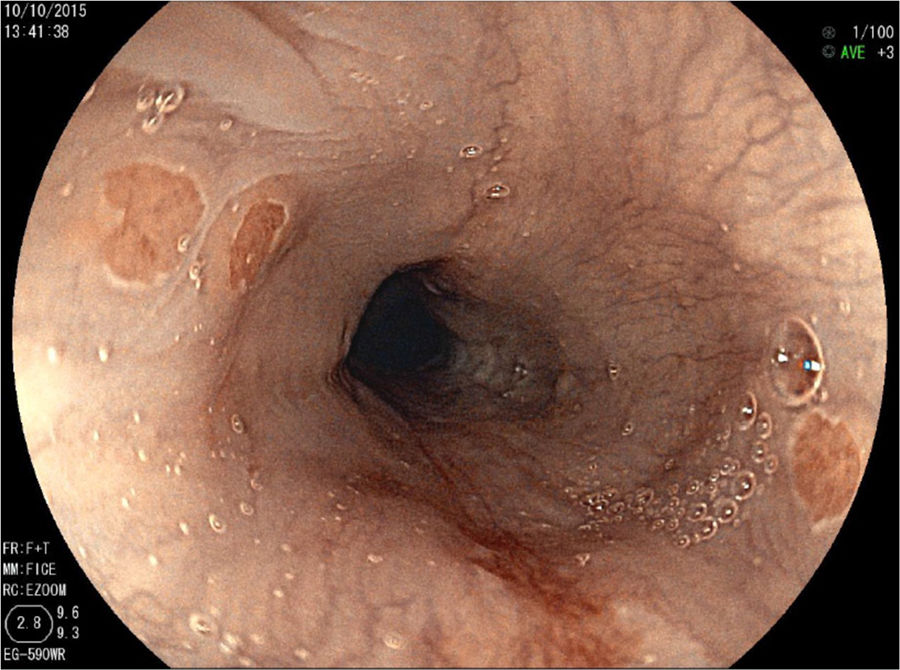
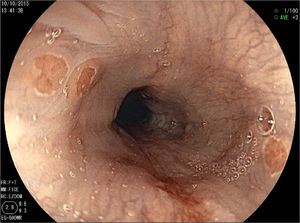
Endoscopic procedureIn all the cases, upper gastrointestinal endoscopy was performed by a single endoscopist accompanied by a researcher. A high-definition endoscope (Fujinon 4450) with an image enhancement system (Fuji intelligent chromoendoscopy, [FICE]) was employed. Intravenous sedation with propofol and midazolam was given by an anesthesiologist. The endoscope was introduced, and the esophagus was carefully examined, paying special attention to its upper third portion and recording the endoscopic findings until reaching the duodenum in all the patients. Upon removing the endoscope, a detailed revision of the upper third of the esophagus was carried out. The endoscope was then reintroduced in FICE mode to re-examine the upper esophagus. If IP was encountered, its morphology was described.
IP was determined as one or more well-delimited, salmon-colored lesions with well-defined margins. The diameter was estimated by comparing the affected area with the diameter of the biopsy forceps. When more than one lesion was found, the lesion with the largest diameter was recorded and two biopsies were taken from each of the suspicious areas.
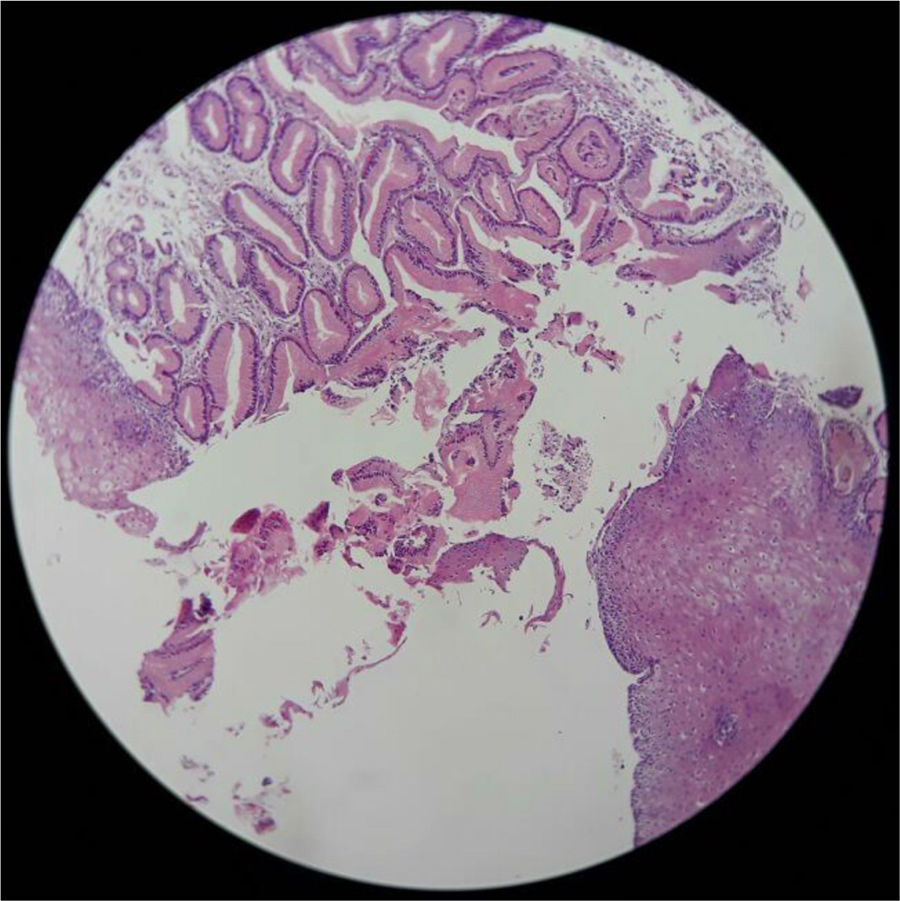
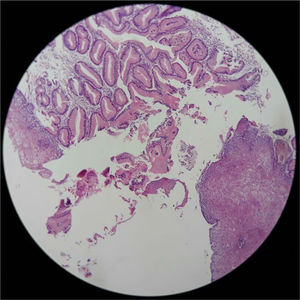
Histopathology studyAll the biopsies were sent to the same pathologist. IP was histologically confirmed when there was glandular gastric columnar epithelium with oxyntic or parietal cells. H. pylori testing was carried out on all patients.
Statistical analysisSample size was calculated using the Epi Info version 7 statistics program (Atlanta, Georgia, USA, 2015), using an expected frequency of 10% and a 99% confidence level. Based on the results, 239 patients were included in the study. Convenience sampling and consecutive patient selection were employed. The chi-square test or Fisher's exact test was used for the correlations and risk was calculated with odds ratio and 95% confidence intervals (95% CI). Statistical significance was set at a p≤0.05.
The present study abided by the international ethics norms, according to the principles stipulated in the World Medical Association Declaration of Helsinki.
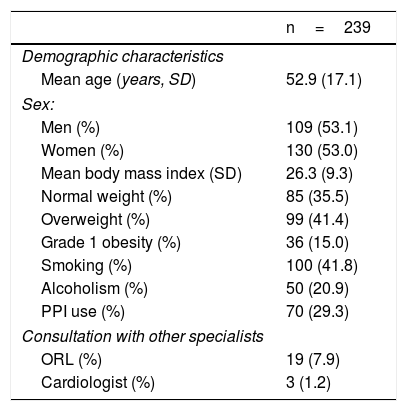
ResultsA total of 239 patients were included in the study, 109 (45.6%) of whom were men and 130 (54.4%), women. Their mean age was 52.9±17.1 years (range: 13-91). table 1 shows the sociodemographic characteristics of the patients and their previous medical consultations with other specialists. The prevalence of IP was 26 (10.9%) patients, 15 of whom were men (57.7%) (table 2 and fig. 1).
Demographic characteristics of the study population.
| n=239 | |
|---|---|
| Demographic characteristics | |
| Mean age (years, SD) | 52.9 (17.1) |
| Sex: | |
| Men (%) | 109 (53.1) |
| Women (%) | 130 (53.0) |
| Mean body mass index (SD) | 26.3 (9.3) |
| Normal weight (%) | 85 (35.5) |
| Overweight (%) | 99 (41.4) |
| Grade 1 obesity (%) | 36 (15.0) |
| Smoking (%) | 100 (41.8) |
| Alcoholism (%) | 50 (20.9) |
| PPI use (%) | 70 (29.3) |
| Consultation with other specialists | |
| ORL (%) | 19 (7.9) |
| Cardiologist (%) | 3 (1.2) |
ORL: otorhinolaryngologist; PPI: proton pump inhibitor; SD: standard deviation.
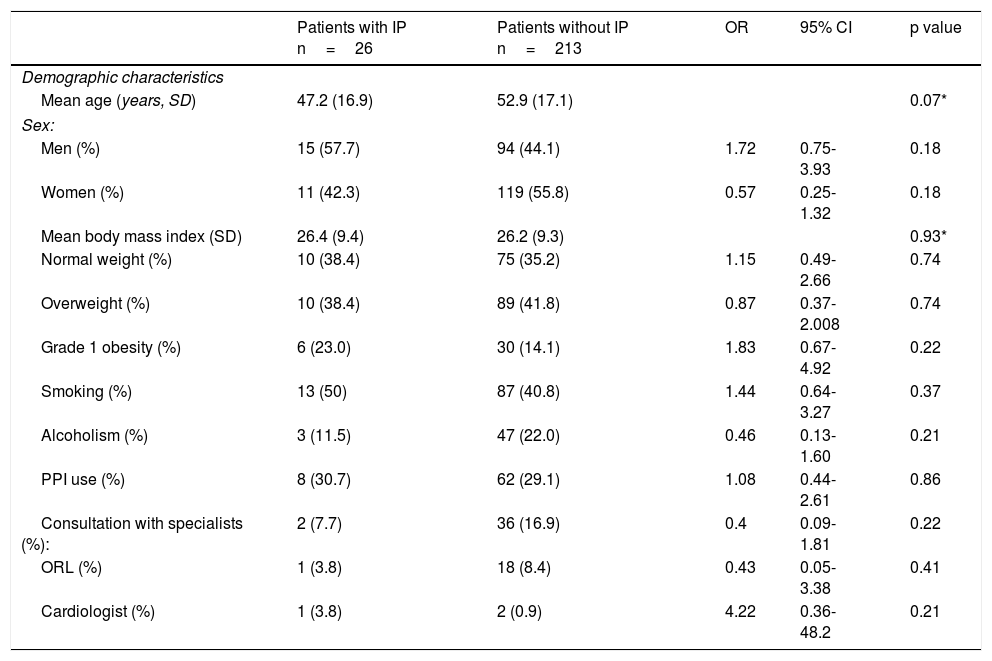
Demographic characteristic in patients with and without inlet patch.
| Patients with IP n=26 | Patients without IP n=213 | OR | 95% CI | p value | |
|---|---|---|---|---|---|
| Demographic characteristics | |||||
| Mean age (years, SD) | 47.2 (16.9) | 52.9 (17.1) | 0.07* | ||
| Sex: | |||||
| Men (%) | 15 (57.7) | 94 (44.1) | 1.72 | 0.75-3.93 | 0.18 |
| Women (%) | 11 (42.3) | 119 (55.8) | 0.57 | 0.25-1.32 | 0.18 |
| Mean body mass index (SD) | 26.4 (9.4) | 26.2 (9.3) | 0.93* | ||
| Normal weight (%) | 10 (38.4) | 75 (35.2) | 1.15 | 0.49-2.66 | 0.74 |
| Overweight (%) | 10 (38.4) | 89 (41.8) | 0.87 | 0.37-2.008 | 0.74 |
| Grade 1 obesity (%) | 6 (23.0) | 30 (14.1) | 1.83 | 0.67-4.92 | 0.22 |
| Smoking (%) | 13 (50) | 87 (40.8) | 1.44 | 0.64-3.27 | 0.37 |
| Alcoholism (%) | 3 (11.5) | 47 (22.0) | 0.46 | 0.13-1.60 | 0.21 |
| PPI use (%) | 8 (30.7) | 62 (29.1) | 1.08 | 0.44-2.61 | 0.86 |
| Consultation with specialists (%): | 2 (7.7) | 36 (16.9) | 0.4 | 0.09-1.81 | 0.22 |
| ORL (%) | 1 (3.8) | 18 (8.4) | 0.43 | 0.05-3.38 | 0.41 |
| Cardiologist (%) | 1 (3.8) | 2 (0.9) | 4.22 | 0.36-48.2 | 0.21 |
IP: inlet patch; ORL: otorhinolaryngologist; PPI: proton pump inhibitor; SD: standard deviation.
The main reason for referral was symptomatic GERD in 18 (69.2%) patients with IP and 119 (55.9%) patients without IP (p=0.19). In relation to endoscopic diagnosis, 6 (23.1%) patients with IP and 49 (23%) without IP presented with Barrett's esophagus (OR: 1.00, CI: 0.38-2.63, p=0.99), and 5 (19.2%) patients with IP and 96 (45.1%) patients without IP presented with hiatal hernia (OR: 0.29, CI: 0.10-0.79, p=0.011). Symptoms typical of reflux were the most common: heartburn in 69.2% of the patients with IP and 59.1% without IP (p=0.32), and regurgitation in 65.4% of the patients with IP and 69.1% without IP (p=0.7). The extraesophageal manifestations that presented were: chest pain in 2 (7.7%) patients with IP and in 2 (0.9%) without IP (OR: 8.78, CI: 1.18-65.28, p=0.8), and globus sensation in 9 (34.6%) patients with IP and in 76 (35.7%) patients without IP (OR: 0.95; CI: 0.40-2.24, p=0.91) (table 3).
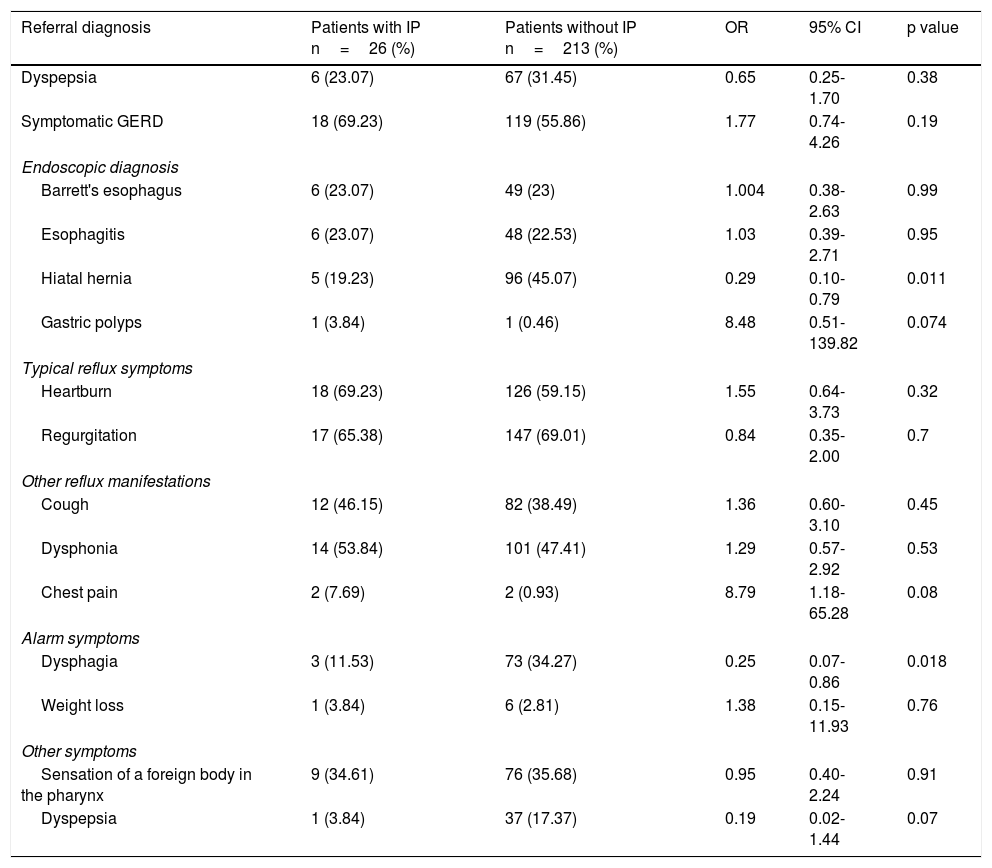
Clinical characteristics of patients with and without inlet patch.
| Referral diagnosis | Patients with IP n=26 (%) | Patients without IP n=213 (%) | OR | 95% CI | p value |
|---|---|---|---|---|---|
| Dyspepsia | 6 (23.07) | 67 (31.45) | 0.65 | 0.25-1.70 | 0.38 |
| Symptomatic GERD | 18 (69.23) | 119 (55.86) | 1.77 | 0.74-4.26 | 0.19 |
| Endoscopic diagnosis | |||||
| Barrett's esophagus | 6 (23.07) | 49 (23) | 1.004 | 0.38-2.63 | 0.99 |
| Esophagitis | 6 (23.07) | 48 (22.53) | 1.03 | 0.39-2.71 | 0.95 |
| Hiatal hernia | 5 (19.23) | 96 (45.07) | 0.29 | 0.10-0.79 | 0.011 |
| Gastric polyps | 1 (3.84) | 1 (0.46) | 8.48 | 0.51-139.82 | 0.074 |
| Typical reflux symptoms | |||||
| Heartburn | 18 (69.23) | 126 (59.15) | 1.55 | 0.64-3.73 | 0.32 |
| Regurgitation | 17 (65.38) | 147 (69.01) | 0.84 | 0.35-2.00 | 0.7 |
| Other reflux manifestations | |||||
| Cough | 12 (46.15) | 82 (38.49) | 1.36 | 0.60-3.10 | 0.45 |
| Dysphonia | 14 (53.84) | 101 (47.41) | 1.29 | 0.57-2.92 | 0.53 |
| Chest pain | 2 (7.69) | 2 (0.93) | 8.79 | 1.18-65.28 | 0.08 |
| Alarm symptoms | |||||
| Dysphagia | 3 (11.53) | 73 (34.27) | 0.25 | 0.07-0.86 | 0.018 |
| Weight loss | 1 (3.84) | 6 (2.81) | 1.38 | 0.15-11.93 | 0.76 |
| Other symptoms | |||||
| Sensation of a foreign body in the pharynx | 9 (34.61) | 76 (35.68) | 0.95 | 0.40-2.24 | 0.91 |
| Dyspepsia | 1 (3.84) | 37 (17.37) | 0.19 | 0.02-1.44 | 0.07 |
IP: inlet patch.
In the 26 patients in whom IP was identified, the mean diameter of the primary lesion was 6.4±3.8mm. A secondary lesion was identified in 14 patients (53.8%), and the mean diameter of those lesions was 4.7±3.3mm (fig. 2).
Three patients with IP had undergone a previous endoscopy at the same endoscopy unit by the same endoscopist, with no resulting diagnosis of IP. In the histopathologic analysis, no dysplasia or H. pylori infection at the IP site was reported in any of the samples and there were no reports of complications of ulcers, bleeding, fistulas, or strictures at that location (fig. 3).
Discussion and conclusionsInlet patch (IP) has been described in different locations, but the proximal esophagus is the most frequent,4,10,11 and is the only site described in the present study.
Prevalence of IP ranging from 1 a 13.8% has been described in various studies,4,12 and is distinct in different populations. A study conducted in Turkey in 2006 by Alagozlu et al. on 6,760 consecutively selected patients referred for upper endoscopy reported a prevalence of IP of 1%, but in 2014, Sahin et al. studied 3,907 patients and found a prevalence of 3.4%,8 coinciding with similar studies on the same population.2,13,14 Likewise, other studies on Japanese patients described a prevalence of 13.8%.15
Prevalence of IP in our study was 10.8%, similar to that reported in other populations.4
The main reasons for endoscopy referral in the present study were symptomatic GERD and dyspepsia, and there was no difference between the patients with or without IP. No association was demonstrated between the presence of a symptom and the presence of IP, similar to results from other studies.16
IP lesions are not often identified or detected. They can easily be missed if the upper esophagus is not carefully examined, resulting in an underestimation of their clinical relevance and prevalence. However, the directed search for IP with new technologies in endoscopy, such as narrow band imaging (NBI) has increased the probability of identifying those lesions, especially if they are small, as shown by Chung et al. They reported an increased prevalence of 11.7% in a group of patients examined through NBI, compared with the 1.9% prevalence in the group not examined through NBI.17 There are no reports in the literature on the use of FICE for identifying IP. In our study, we carried out a directed search with FICE in all the patients, identifying 3 new patients with IP. They had undergone a prior endoscopic study not longer than 12 months earlier, performed by the same endoscopist with the same equipment, in which no IP was found. Therefore, we believe that a directed search and the use of digital chromoendoscopy increase the possibility of identifying IP.
The clinical manifestations of IP and their importance are subjects of debate. The majority of patients have been described as asymptomatic or having symptoms associated with reflux, such as globus sensation,18 heartburn, regurgitation, and dysphagia.4,16–19 We had similar results, with heartburn identified in 18/26 patients with IP and regurgitation in 17/26 patients with IP, but with no differences in relation to patients without IP (p > 0.3 and p=0.7, respectively). Dysphagia was recorded in 3 patients with IP and in 73 patients without IP, with a significant difference (p=0.018), similar to that reported in the United States by Govani et al. in a study on 822 patients. They found no association between IP and the symptoms of reflux, globus sensation, or dysphagia.20
In a Japanese study that included 2,116 patients, the authors reported that globus sensation was more highly associated with GERD than with IP.15 In the present study, 9/26 patients with IP and 76 /213 without IP (p=0.91) presented with the sensation of a foreign body (globus).
We found no complications such as those described in the literature: dysphagia, strictures, ulcers, tracheoesophageal fistula, esophagocutaneous fistula, esophageal perforation, polyps, membranes, bleeding, premalignant conditions, and even inlet patch-associated carcinomas.7,8,16,21
The inlet patch can be unique or accompanied by mirror or satellite lesions.13,22 In our study, 14 patients (53.8%) had multiple lesions. The mean size of the primary lesion was 6.46±3.85mm and the mean diameter of the satellite lesions was 4.7±3.3mm.
A clinicopathologic classification has been suggested that categorizes the entity into 5 groups, depending on the clinical, endoscopic, and histopathologic characteristics. Class I: patients are asymptomatic and have no other endoscopic finding, class II: patients are symptomatic and present with laryngopharyngeal reflux, class III: patients are symptomatic and have associated complications such as fistulas, bleeding, strictures, or membranes, class IV: there is intraepithelial dysplasia, and class V: there is malignant transformation and patients are asymptomatic or present with dysphagia.4,14,21
In the present study, all the patients with IP (n=26) presented with esophageal and extraesophageal symptoms and had no complications, dysplasia, or malignant findings. Thus, their clinicopathologic classification was class II.
Different studies have described the capacity of the heterotopic gastric mucosa to produce acid.4,17,23 In the Colombian study by Castaño et al., they demonstrated the capacity of the IP to produce acid and extraesophageal manifestations characteristic of gastroesophageal reflux disease and complications. They did not find a unique acid secretion pattern, given that acid was produced both during the day and at night.1
The presence of H. pylori has been reported in IP biopsies.1,8,9 In our study, all of the IP biopsies were negative for the bacterium, coinciding with the results described by Weickert et al. in which 33 patients with inlet patch were negative for said infection.13,24
Ablation with radiofrequency has been described as treatment for IP in symptomatic patients, if the lesions are small. If the lesions are larger than one-third of the circumference, they can be treated with argon plasma coagulation, albeit a possible complication of that procedure is stricture. Dunn et al. treated 10 symptomatic adult patients with radiofrequency ablation and after 2 sessions, 8 of the 10 patients showed complete histologic and endoscopic remission of the heterotopic gastric mucosa, with no signs of any adverse event. Up to 80% of patients that undergo radiofrequency ablation have shown symptom remission. Klare et al. treated 31 symptomatic adult patients with argon plasma coagulation. Resolution was achieved, with no signs of adverse events, in 23 of the 31 patients treated.25 It should be emphasized that those results are from case series.
In conclusion, the prevalence of inlet patch was high in our environment, at 10.9%. Directed search and the use of new technologies (FICE or NBI) can increase IP detection. No significant association with any type of symptom was demonstrated.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: López-Colombo A, Jiménez-Toxqui M, Gogeascoechea-Guillén PD, Meléndez-Mena D, Morales-Hernández ER, Montiel-Jarquín ÁJ, et al. Prevalencia y características clínicas de pacientes con parche de mucosa gástrica ectópica en esófago. Revista de Gastroenterología de México. 2019;84:442–448.