Antecedentes: La impactación esofágica por bolo alimenticio es un síntoma de debut en pacientes diagnosticados de esofagitis eosinofílica, lo cual supone un cambio en la epidemiología y el manejo de esta urgencia.
Objetivo: Detectar factores predictores de esofagitis eosinofílica en pacientes con impactación esofágica por bolo alimenticio.
Métodos: Se analizaron de forma retrospectiva pacientes atendidos por impactación por cuerpo extraño. Se estudiaron las características epidemiológicas, los hallazgos endoscópicos y los antecedentes de impactación. El análisis estadístico se realizó mediante los test de la t de Student y de la χ2. Se elaboró un modelo de regresión logística.
Resultados: Ciento treinta y un pacientes, 65% varones, con una edad media de 56 años. En los pacientes con impactación por bolo alimenticio (n = 89), la sospecha endoscópica de esophagitis eosinofílica fue el hallazgo más frecuente. De estos, aquellos sin confirmación histológica fueron excluidos (n = 7); el resto de los pacientes (n = 82) se dividió en 2 grupos: esofagitis eosinofílica confirmada (grupo A) (n = 18) y otros hallazgos endoscópicos (grupo B) (n = 64). El grupo A presentaba una menor edad media (36.47 vs. 64.45; p = 0.001) e historia de impactación previa más frecuente que el grupo B (38 vs. 6%; OR = 15.70; IC del 95%, 3.60-62.50; p = 0.001). Edad e historia de impactación se comportaron como predictores de esofagitis eosinofílica con una sensibilidad del 82%, una especificidad del 80% y un rendimiento del 84% (p < 0.001).
Conclusión: Edad y antecedentes de impactación predicen la presencia de esofagitis eosinofílica en pacientes con impactación por bolo alimenticio.
Background: Food bolus esophageal impaction is often the first symptom in patients diagnosed with eosinophilic esophagitis, representing a change in the epidemiology and management of this urgency.
Aim: To detect eosinophilic esophagitis predictive factors in patients with esophageal impaction due to food bolus.
Methods: Patients seen for foreign body impaction were retrospectively analyzed. Epidemiologic characteristics, endoscopic findings, and impaction history were studied. The statistical analysis was carried out using the Student's t test and the chi square test and a logistic regression model. Results: Of the 131 patients, 65% were men and the mean age was 56 years. The endoscopic suspicion of eosinophilic esophagitis was the most frequent finding in patients with food bolus impaction (n = 89); those patients that did not have histologic confirmation were excluded (n = 7). The remaining patients (n = 82) were divided into two groups: confirmed eosinophilic esophagitis (Group A) (n = 18) and other endoscopic findings (Group B) (n = 64). Group A presented with a lower mean age (36.47 vs. 64.45, P=.001) and a more frequent past history of impaction (38% vs. 6%, OR = 15.70, 95% CI (3.60-62.50), P=.001) than Group B. Age and impaction history acted as predictors for eosinophilic esophagitis with 82% sensitivity, 80% specificity, and 84% diagnostic accuracy (P<.001).
Conclusions: Age and a history of impaction predict the presence of eosinophilic esophagitis in patients with food bolus impaction.
Introduction
The majority of foreign bodies (FBs) that are impacted in the upper digestive tract are spontaneously resolved, but between 10 and 20% of them require medical attention, and surgery is necessary in 1%. Fortunately, the mortality rate is extremely low.1-5 Over the last few years there has been a significant increase in the number of impaction episodes in young patients, and eosinophilic esophagitis (EoE) has been the main cause.6 Nevertheless, food bolus impaction is one of the most frequent symptoms (25-100%) in EoE patients.7 This new setting can mean a change in epidemiology and urgent endoscopic FB impaction management, taking into consideration that EoE conditions an increase in the risk for complications during the endoscopic procedure, especially esophageal tears and perforations.
The aim of the present study was to analyze the demographic characteristics of the patients seen at our unit for FB impaction, paying special attention to those with endoscopic findings suggestive of EoE (the presence of esophageal rings, linear furrows, white exudates, reduced caliber of the esophageal lumen), in an attempt to detect predictive factors of the disease to aid in preventing complications during endoscopy.7
Methods
Patient selection
A retrospective analysis was done on 131 patients seen at our endoscopy unit for FB impaction over a period of 2 years (from January 1, 2009 to December 31, 2010). Patients with a previously known esophageal pathology or a history of cardiopulmonary pathology were not excluded from the analysis. All patients underwent a 2¿dimensional neck x¿ray, as well as abdominal and chest films, in order to rule out possible complications that would contraindicate endoscopy.
Endoscopic procedure
All patients underwent endoscopic exploration under conscious sedation within the first 6 hours of their arrival at the Emergency Service. The impaction removal procedure was performed using the therapeutic arsenal available at the unit (polypectomy snare, Roth Net foreign body retriever, foreign body forceps, Dormia basket). They were introduced through the working channel of the endoscope (GIF-Q160 Olympus, Hamburg, Germany). The therapeutic aim was the removal of the FB, but it became technically impossible at times. Therefore the bolus was fragmented and moved toward the stomach by means of insufflation and slight pressure with the tip of the endoscope. This technique has been described in the latest consensus guidelines of the American Society of Gastrointestinal Endoscopy (ASGE) published in 2011.3
The exploration data were obtained from the unit's database (Software Endobase Olympus, Hamburg, Germany).
The patients with endoscopic findings that raised suspicion for EoE (ringed esophagus, linear furrows, white plaques, reduced caliber of the esophageal lumen) were referred to the outpatient service for the completion of the study and they were analyzed independently. Epidemiologic characteristics, endoscopic findings, type of foreign body, impaction history during the 3 years prior to the analysis, and the time of year in which episodes occurred were all studied. The medical records were reviewed for clinical and histologic EoE criteria.6 Those patients that did not have a confirmation diagnosis were scheduled for a second endoscopy in which at least 5 biopsies were taken from the esophagus by segments (distal and proximal) using the conventional biopsy forceps (Boston Scientific¿Costa Rica, Radial JawTM 4, Propack). Patients with no available medical record were interviewed by telephone and asked about symptomatology suggestive of EoE.
Histologic analysis
The biopsy specimens were sent to the Pathologic Anatomy Service, where they were fixed in formalin and embedded in paraffin. Serial sections 3 to 5 μ thick were cut with a microtome, stained with hematoxylin and eosin, and then examined under an optic microscope (Nikon®g; Eclipse 80i microscope). The samples were also stained with PAS to rule out the presence of fungi. Diagnosis "histologically consistent with EoE" was made when more than 15 eosinophils per high power field (x40) were detected, and especially when the eosinophilic infiltrate prevailed in the upper layers of the epithelium, forming aggregates (micro-abscesses).
Study design
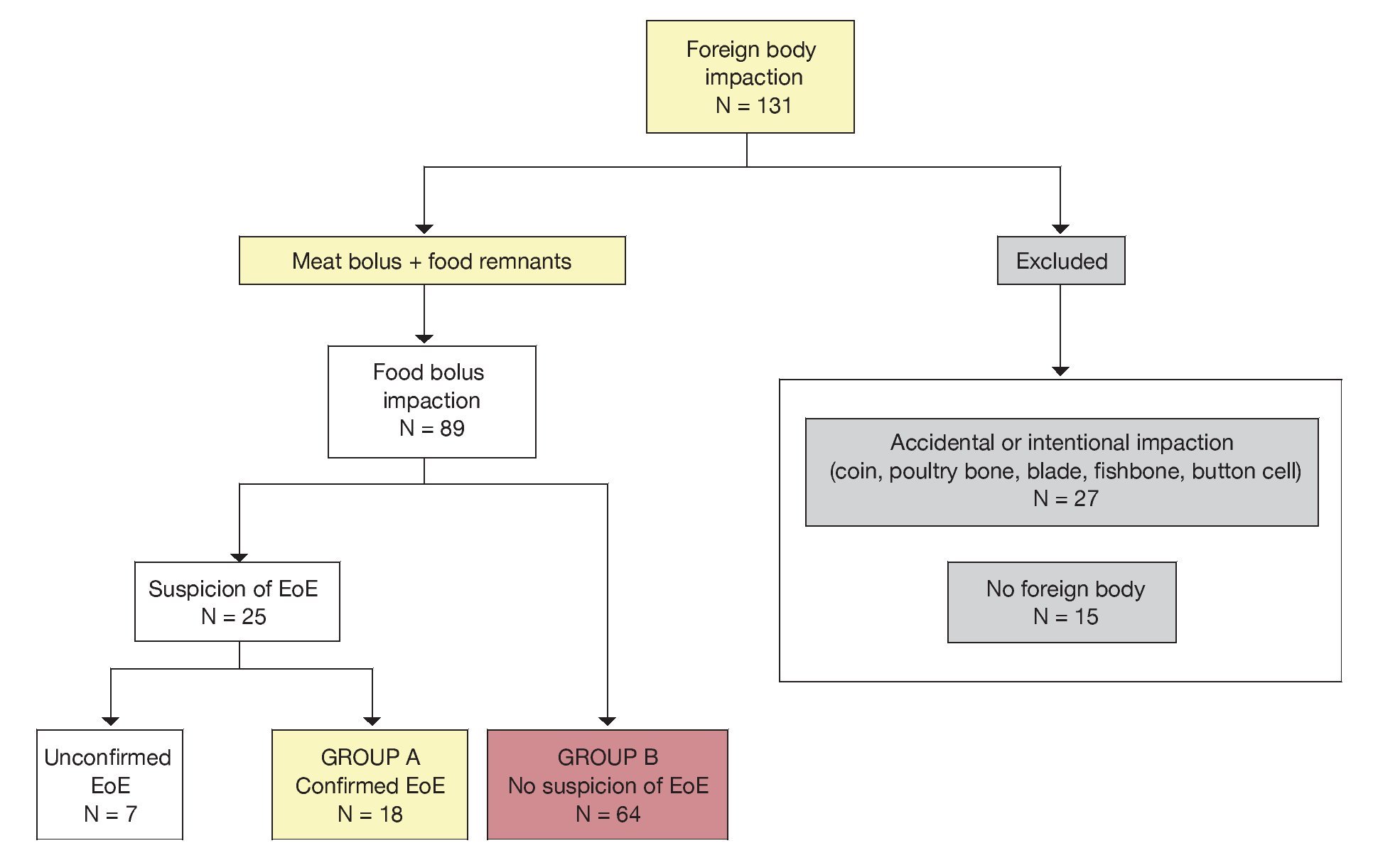
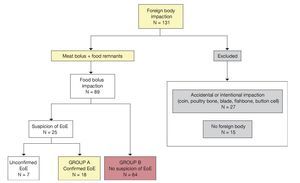
Those subjects with «traumatic» impaction (bones, coins, button cells, blades) (20%, 27/131), those that did not present with FB impaction (11.4%, 15/131), and the group of subjects that had findings suggestive of EoE, but that were not histologically confirmed (5%, 7/131) were excluded from the analysis. For the remaining population (n=82), a case-control study was designed with a retrospective data source, dividing the sample into two subgroups: group A (endoscopic findings suggestive of EoE that were histologically confirmed, n=18) and group B (other endoscopic findings, n=64) (Fig. 1).
Figure 1. Study design.
Statistical analysis
A database was constructed using Microsoft Access 2007 and the SPSS v.18 (PASW18) statistical package. The Student's t test and chi square tests were employed and a binary logistic regression model was applied from the multivariate analysis. Statistical significance was set with an α error ≤ 0.05. The sensitivity and specificity of the model were represented through ROC curves.
Results
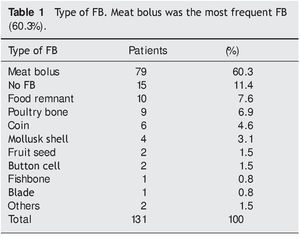
The analysis was done on 131 patients (85 men and 46 women) with FB impaction that were seen at our unit over a 2-year period (from January 1, 2009 to December 31, 2010). The mean age was 56 years (1-99 years) and 14 patients were under the age of 18 years. After upper gastrointestinal hemorrhage, FB impaction was the most frequent endoscopic urgency (24%, 131/536). According to information published by the Health Department of Castilla-La Mancha (SESCAM), our health zone has a population of 250,000 inhabitants,7 with an estimated FB impaction incidence of 33 cases/100,000 inhabitants per year.
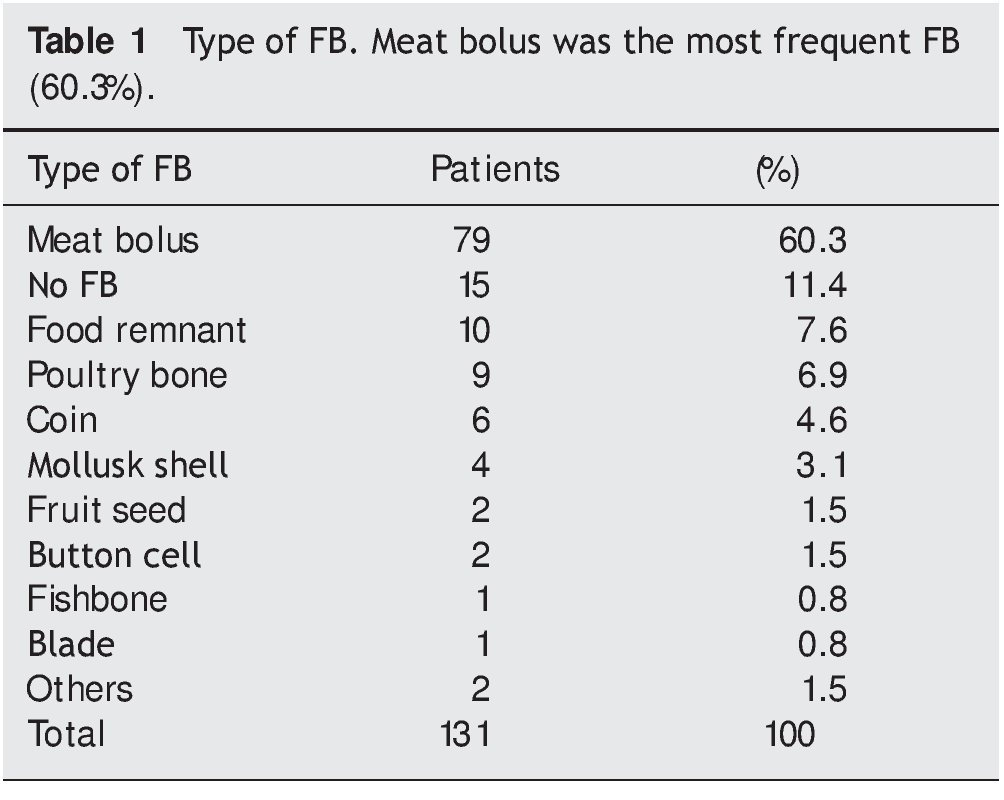
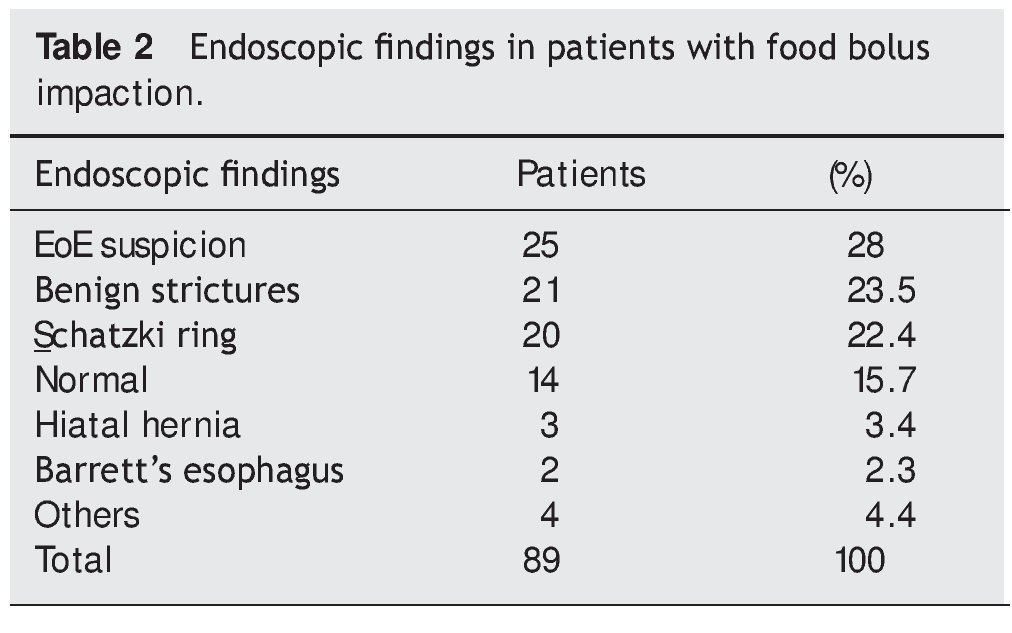
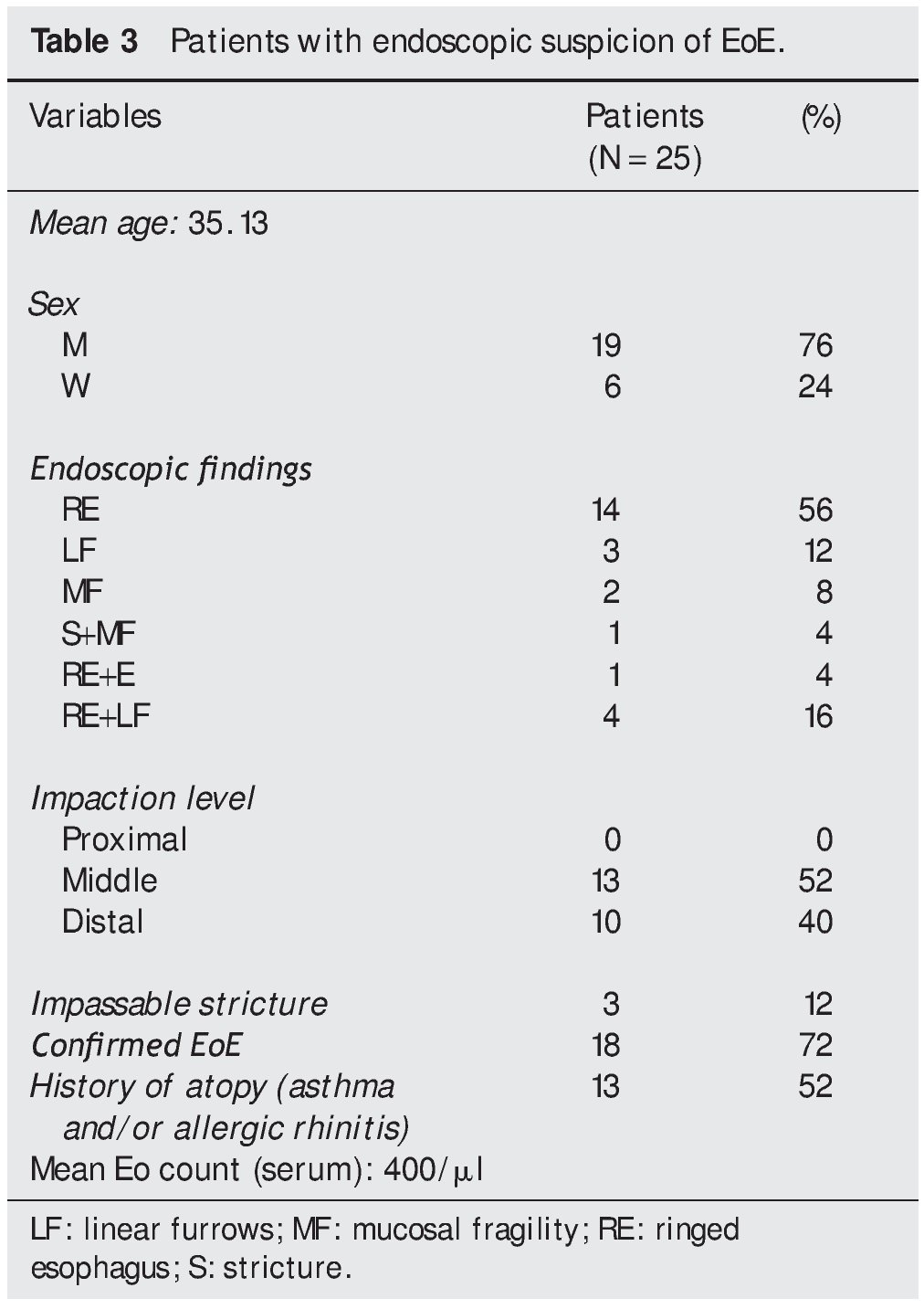
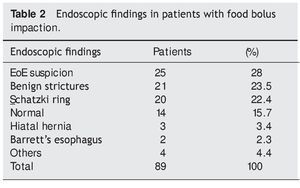
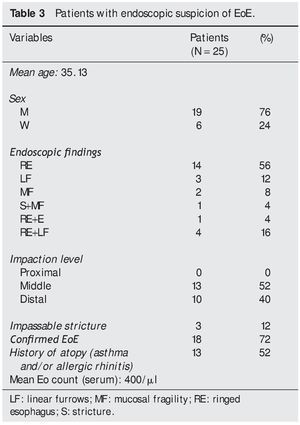
No FB was found in 11.4% of the cases (15/131) and when it was found, the most frequent FB was a meat bolus (60.3%, 79/131) (Table 1). Normal endoscopy was the most frequent finding (34.4%; 45/131). Among the pathologic findings, Schatzki ring was the most frequent (19.8%, 26/131), followed by findings suggestive of EoE (19%, 25/131). No neoplastic lesions were found as the cause of impaction. When patients with food bolus impaction (meat or food remnants) (89/131) were analyzed, endoscopic suspicion of EoE was observed to be the most frequent finding (28%, 25/89) (Table 2). The majority of patients presented with ringed esophagus in the endoscopy (56%, 14/25) (Table 3). Therapeutic success was achieved (impaction removal rate) in 98.3% of the cases (114/116) with no complications during the procedures. The FB was recovered in 59.4% of the cases (69/116). Impaction removal was carried out in the remaining patients through the technique of pushing and fragmenting the bolus with the tip of the endoscope, moving it toward the stomach. The impaction was unable to be endoscopically removed in two cases and the help of an otorhinolaryngologist was requested.
Endoscopic urgency due to FB impaction was more frequent in 2009 than in 2010 (36% vs. 21%, p=0.02).
EoE diagnosis was confirmed in 72% of the patients (18/25). The rest of the patients (7/25) did not continue with follow-up in our service and so 42% (3/7) of them were interviewed by telephone, and referred to the persistence of dysphagia symptoms.
There was a seasonal tendency in the appearance of findings that were suggestive of EoE; 68% (17/25) of them were found between April and September but this tendency was not statistically significant (p=0.49; OR=1.50; 95% CI, 0.47 to 4.76).
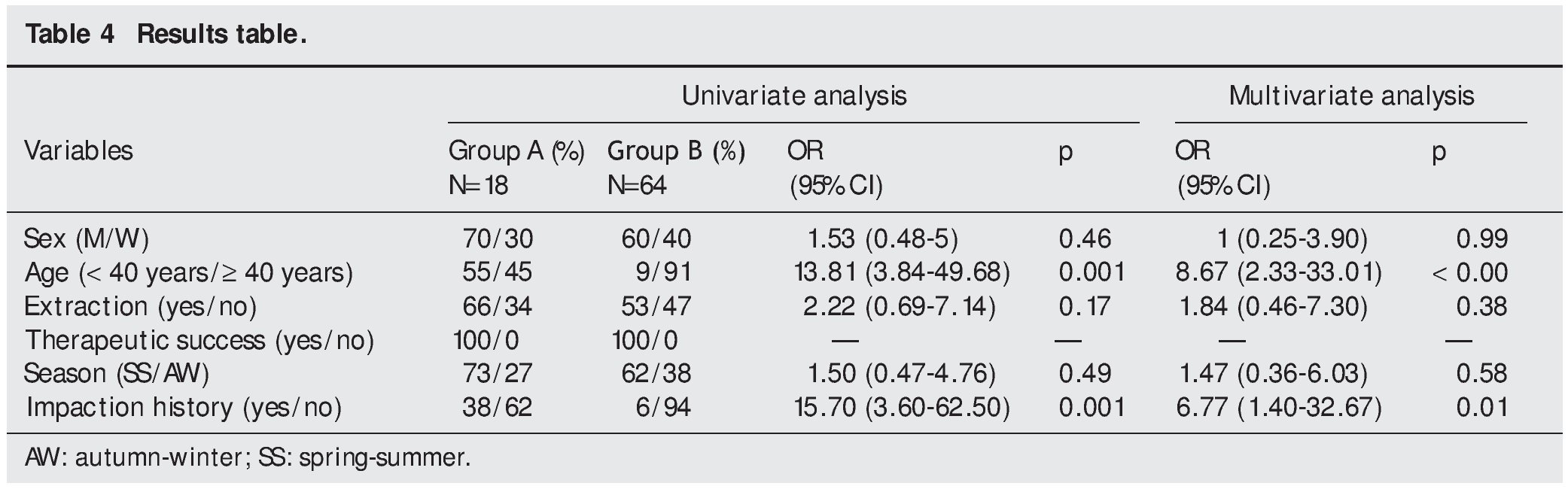
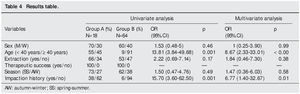
In the comparative analysis of the two cohorts (group A and group B), the results were as follows (Table 4): in relation to sex, there was a greater percentage of men in group A than in group B, but the difference was not statistically significant (70% vs. 60%, p=0.46; OR=1.53; 95% CI, 0.48 to 5). The mean age in group A (36.47 years; 15-85) was significantly lower than in group B (64.45 years; 2¿99), (p=0.001). Transforming age into a dichotomic variable and establishing 40 years as the cut-off point, 55% of the subjects in group A were under that age, as opposed to only 9% in group B (p=0.001; OR=13.81; 95% CI, 3.84-49.68). In regard to impaction history, 38% of the group A patients referred to prior episodes compared with 6% of the group B patients (p=0.001; OR=15.70; 95% CI, 3.60-62.50). There were no statistically significant differences in regard to FB extraction rate (66% [A] vs. 53% [B]; p=0.17), nor in relation to therapeutic success (impaction removal rate), which was 100% in both groups. No differences were found in reference to seasonal tendency between one group and the other.
Multivariate analysis and binary logistic regression
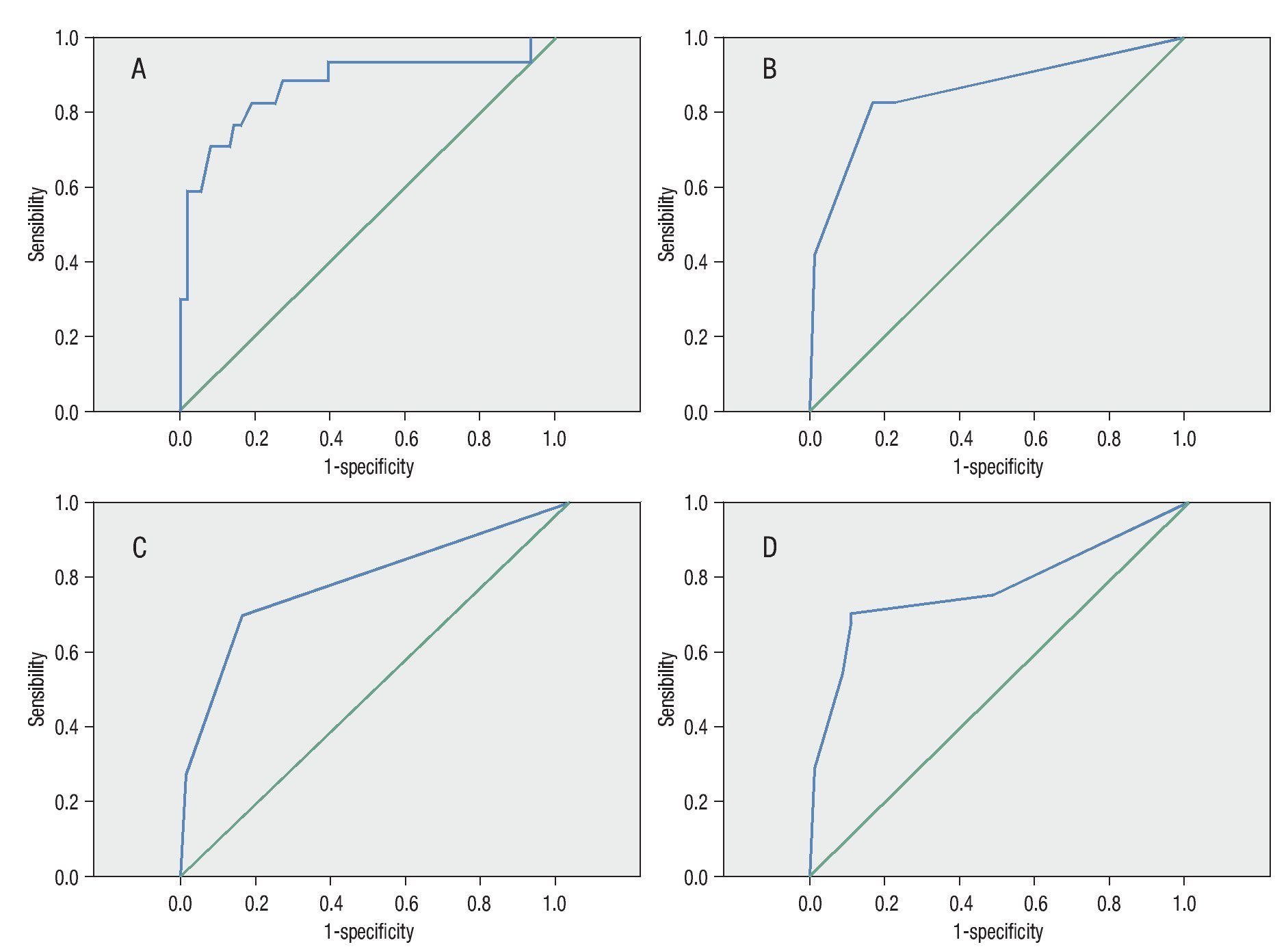
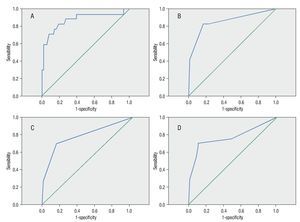
In the multivariate analysis, age (p<0.001) and previous impaction history (p=0.01) were found to be independent predictors of endoscopic findings suggestive of EoE. A binary logistic regression model was constructed with these two variables that had 82% sensitivity, 80% specificity, and 84% diagnostic accuracy (p<0.001) for predicting endoscopic findings suggestive of EoE. These data were expressed through ROC curves with an area under the curve (AUC) of 0.86 (Fig. 2).
Figure 2. ROC curves. Binary logistic regression. A) Age and previous impaction history (AUC: 0.86, S: 82.4%, Sp: 80%). B) Age (
Discussion
FB impaction is the second most frequent endoscopic emer gency1 in the developed countries, and this concurs with the results of our study. Incidence was 33 cases/ 100,000 inhabitants per year. This figure is significantly higher than that published in the literature, in which the incidence is from 13 to 20 cases/100,000 inhabitants per year.9,10 In fact, geographic area has been observed to have an influence on FBs and more specifically on food bolus impaction.9,11 This can explain the discrepancies in the incidence figures, but no studies have been conducted on FB impaction in our environment that can serve as a reference. The mean age of patients was 56 years, similar to previously published data.6,12,13 Meat bolus was the most frequent FB at 60.3% (79/131), concurring with that published in recent series in which there was an estimated frequency of 42.7% and 65%.12,13 The most frequent endoscopic finding was the Schatzki ring (19.8%, 26/131), with no symptoms complained of in 34.4% of the cases (45/131). However, if we exclude the subjects with traumatic impaction (bones, coins, button cells, blades), then EoE suspicion becomes the most frequent endoscopic finding (28%, 25/89).
According to the latest EoE consensus guidelines published in 2011,14 EoE is defined as a chronic, immune/ antigen-mediated esophageal disorder characterized by symptoms of esophageal dysfunction and a predominantly eosinophilic inflammatory infiltrate. The main symptom in adult patients is dysphagia, which presents in 11 to 100% of the patients,15 whereas food bolus impaction occurs in 33 to 54% of the cases.16 Nevertheless, various studies have shown the presence of EoE in 20 to 54% of the patients presenting with food bolus impaction.6,12,16
In our study, we found 25 patients with endoscopic suspicion of EoE, and the disease was histologically confirmed in 18 of them.8 EoE could not be confirmed in the other 7 patients due to a lack of biopsies. It was striking that dysphagia symptoms continued in 3 of the 7 patients, leading to the strong suspicion of EoE. There was no further information on the 4 remaining patients because they had no follow¿up. Endoscopic findings suggestive of EoE are not pathognomonic of the disease.17-19 As a matter of fact, there are studies in which no close relation between EoE suspicion and histologic results have been found. For example, in a published study by Prasad et al.,20 only 8 out of 21 patients with endoscopic suspicion of EoE had a confirmed presence of >20 eosinophils per high power field, even though they employed a larger cut-off point than that currently used by consensus (>15 eosinophils per high power field). This report highlights the most important limitation of our study: because ours was a retrospective analysis, biopsies of all patients were not available to us, and together with the high rate of normal endoscopies, it is possible that our results could be underestimated.
On the other hand, Straumann et al.21 found a positive correlation between the endoscopic findings (white exudates) and the number of eosinophils found in biopsies and dysphagia episode frequency.
In addition, there are studies that suggest the existence of motor disorders associated with eosinophilic infiltration in the esophageal wall,22,23 which can explain the different disease manifestations (dysphagia, food bolus impaction, etc.).
In published case series,11,23 no endoscopic evidence of impaction was found in a significant number of patients suspected of having food bolus (15.6% in our study). This is probably due to the amount of time that elapsed from the impaction event to the performance of the endoscopy (a datum not analyzed in our study).
Due to the fact that EoE can present with no endoscopic manifestations,14,24,25 it is possible that it is under-diagnosed as a cause of food bolus impaction. In fact, in the study published by Katsinelos et al.,24 the histologic results in 3 of the 8 patients that presented with normal endoscopy were consistent with EoE, once again underlining the most important limitation of our study.
Following this line of thought, Kirchner et al.12 recently published a study in which they took biopsies from 48 patients with food bolus impaction and found that 10 of them had eosinophilic infiltration. Desai et al.16 had similar results in a recent study that were confirmed by Kerlin et al.6
The estimated cut-off point of more than 15 eosinophils per field is still somewhat controversial. Ravi et al.26 recently published a study in which they found no differences in relation to endoscopic findings and clinical manifestations in patients with <15 eosinophils per field compared with a group of patients with >15 eosinophils. This finding has resulted in the coining of the term «low grade eosinophilic esophagitis» for those cases in which clinical and endoscopic presentations are consistent with EoE but there are fewer than 15 eosinophils per field in the biopsies.26,27
In our case series, we did not have the exact count of eosinophils per field due to the fact that the pathologic anatomy reports in which there were more than 15 eosinophils were classified as consistent with EoE. All these studies underscore the importance of disease suspicion in patients with food bolus impaction. This is why we designed a logistic regression model to help predict the presence of disease in the context of this endoscopic urgency, in which age and a previous impaction history were the most important EoE predictive factors, with an 82.4% sensitivity and an 80% specificity. This enabled us to suspect disease with a high accuracy rate prior to the performance of endoscopy, even when endoscopy was normal.
It is a known fact in EoE that the esophagus suffers a loss of elasticity, increasing the risk for complications during endoscopy.28-30 Serum markers such as IgE and serum levels of eosinophils can be helpful in relation to disease suspicion, but more prospective studies are needed to prove this fact.31 In our study, we found that in the 13 patients with endoscopic suspicion of EoE, there was a prior history of atopy (allergic rhinoconjunctivitis, bronchial asthma, atopic dermatitis), representing 52% of the total (Table 3). This aspect could act as a predictive factor of the disease, but because our study was retrospective, we could not collect this datum in the comparison group (group B). Early disease suspicion, even before endoscopy, aids in the prevention of complications and in the selection of patients that can benefit from a first disease screening through biopsy during urgent endoscopy.
In conclusion, EoE is a clinical entity that is becoming more and more frequent in patients seeking medical attention for food bolus impaction. Age (especially when under 40 years) and a prior history of impaction can help us predict the disease, enabling early diagnosis and the avoidance of complications during endoscopy.
Financial disclosure
No financial support was received in relation to this article.
Conflict of interests
The authors declare that there is no conflict of interest.
Received 9 July 2012; accepted 9 October 2012
Available online 29 January 2013
qPlease cite this article as: Rodríguez-Sánchez J, et al. Factores predictores de esofagitis eosinofílica en impactación esofágica por bolo alimenticio. Revista de Gastroenterología de México. 2013;78:5-11.
* Corresponding author at:
Hospital General Universitario, C/ Obispo Rafael Torija s/n, 13005 Ciudad Real, Spain.
Email address:joarosa@sescam.jccm.es (J. Rodríguez-Sánchez).