Primary colorectal lymphomas are a rare disorder, corresponding to 0.05% of all colonic neoplasias and 0.1% of primary tumors of the rectum.1,2 Plasmablastic lymphoma (PL) is a very rare subtype of diffuse large B-cell lymphoma (DLBCL),3 defined by the WHO as a “diffuse proliferation of large cells, the majority of which resemble B cells, but have a plasmacytic immunophenotype”.4 It has distinctive pathologic and clinical characteristics, such as the absence of CD20 expression, positivity for Epstein-Barr virus, an aggressive clinical course, and a close association with the human immunodeficiency virus (HIV). It usually affects the oral cavity but has recently been reported in other extraoral sites.5 It involves the gastrointestinal tract in 14% of patients and very few cases of rectal involvement have been reported.6
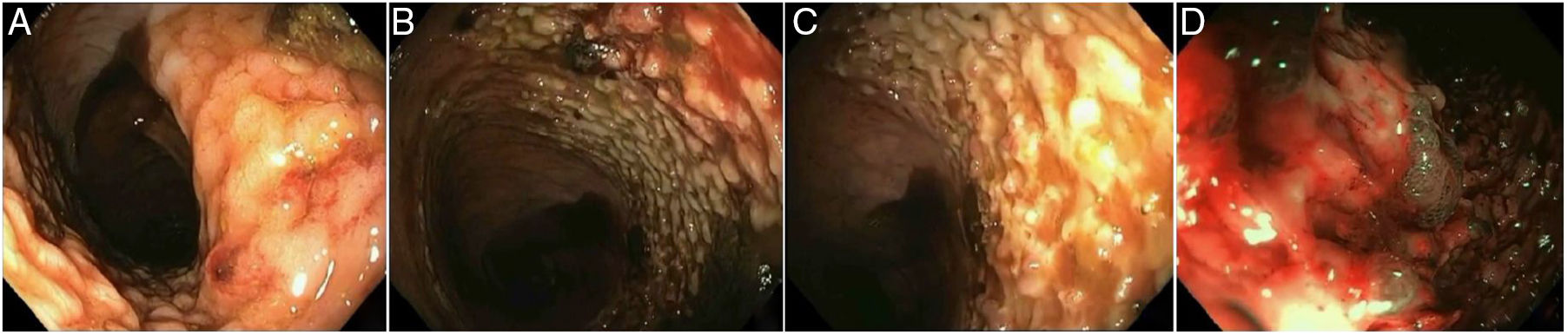
We present herein the case of a female patient with PL. A 58-year-old woman with a history of morbid obesity and peripheral venous insufficiency arrived at the emergency service due to deep vein thrombosis in the left leg, associated with phlebitis and severe sepsis. During her hospitalization, she presented with hematochezia that caused hypovolemic shock. Rectosigmoidoscopy revealed a lesion in the rectum that was large, granular, flat, raised, and growing laterally (fig. 1A) that affected 75% of the circumference of the rectum. The superficial mucosa was whitish (fig. 1B and C) with stigmata of recent hemorrhage: multiple small clots adhered to the lesion (fig. 1D). Abdominopelvic tomography showed no intra-intestinal or distant tumor activity.
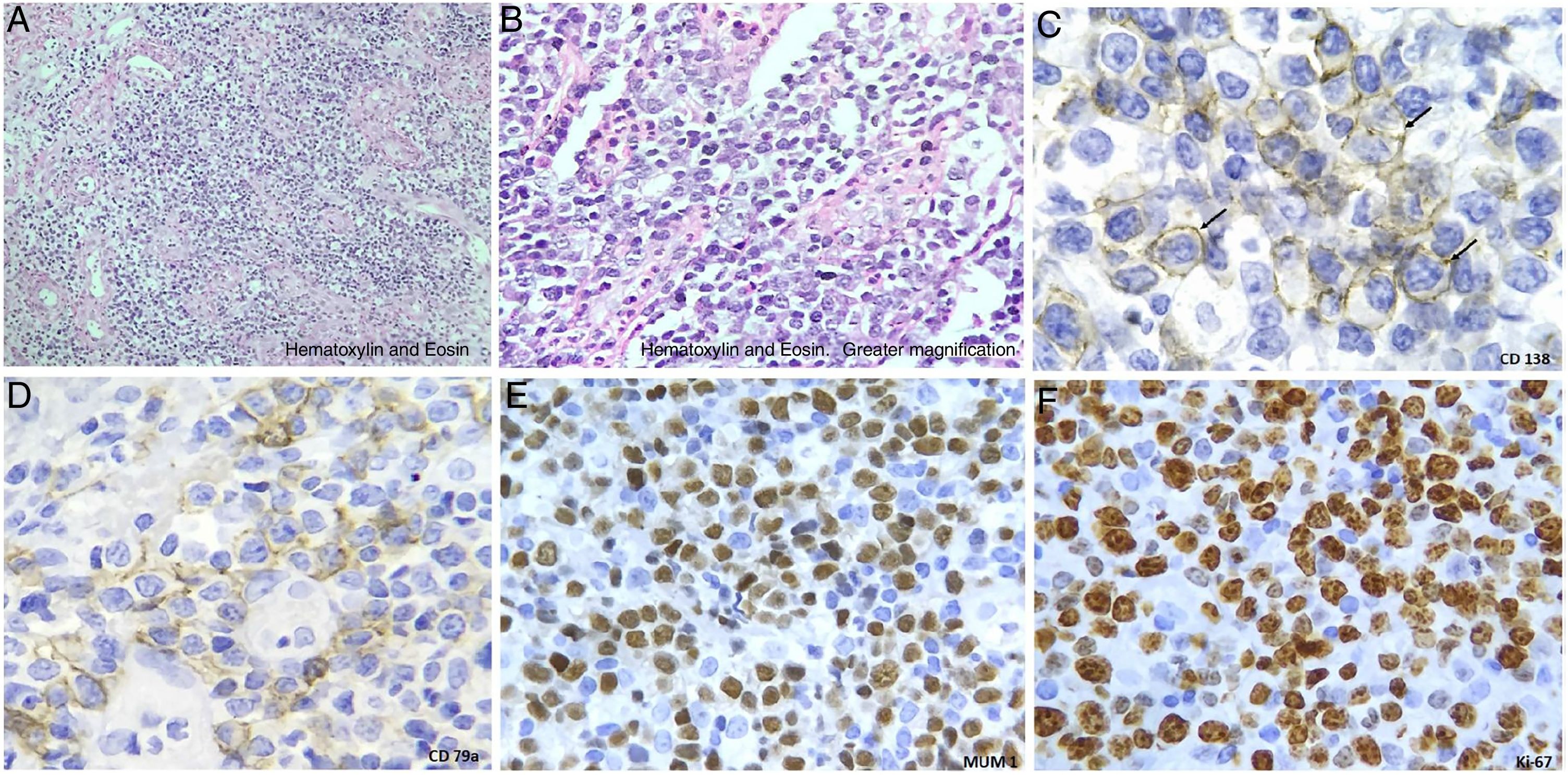
In the hematoxylin and eosin (H&E) staining of the biopsies taken during the endoscopic study, neoplastic cells mixed with small mature lymphocytes were observed (fig. 2A and B) . Non-Hodgkin's lymphoma was originally reported, for which immunohistochemical staining was carried out. The tumor cells stained positive for CD138 (plasmatic cell membrane marker), CD79a (immature B-cell marker), MUM1 in the nuclei of the tumor cells, and Ki-67 (90%), establishing a high proliferation rate of neoplastic cells (fig. 2C-F). The complete immunohistochemistry panel included: positive Epstein-Barr encoding region (EBER) performed through in situ hybridization; positive, focal, and weak Bcl-6; and negative ALK-1, HHV-8, CD20, CD3, Bcl-2, CD5, and CD56. The report's conclusion was plasmablastic lymphoma.
The clinical course was aggressive, with persistence of the septic focus (Pseudomonas aeruginosa was isolated) and bleeding recurrence. The patient died 30 days after hospital admission due to hypovolemic and septic shock. The diagnosis was made post mortem and it was not possible to look for HIV infection.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Pérez-Mendoza A, Zárate-Guzmán AM, Lázaro-Pacheco IB, Navarrete-Pérez JJ. Linfoma plasmablástico de recto. Causa poco frecuente de hemorragia digestiva baja: reporte de un caso. Revista de Gastroenterología de México. 2019;84:519–520.