Meckel's diverticulum (MD) is a vestigial remnant of the omphalomesenteric duct that consists of a saccular dilation of the small bowel, located at the antimesenteric border, generally at fewer than 60-100cm from the ileocecal valve. It is the most common malformation of the small bowel and has a prevalence of 2-3%. Symptomatic MD is more frequent in males than in females.1 It is composed of all the bowel wall layers and therefore is a true diverticulum. Up to 60% of the cases can present with heterotopic tissue of the gastric, pancreatic, colonic, or duodenal mucosa.2
We present herein an unusual case of MD perforated by a foreign body.
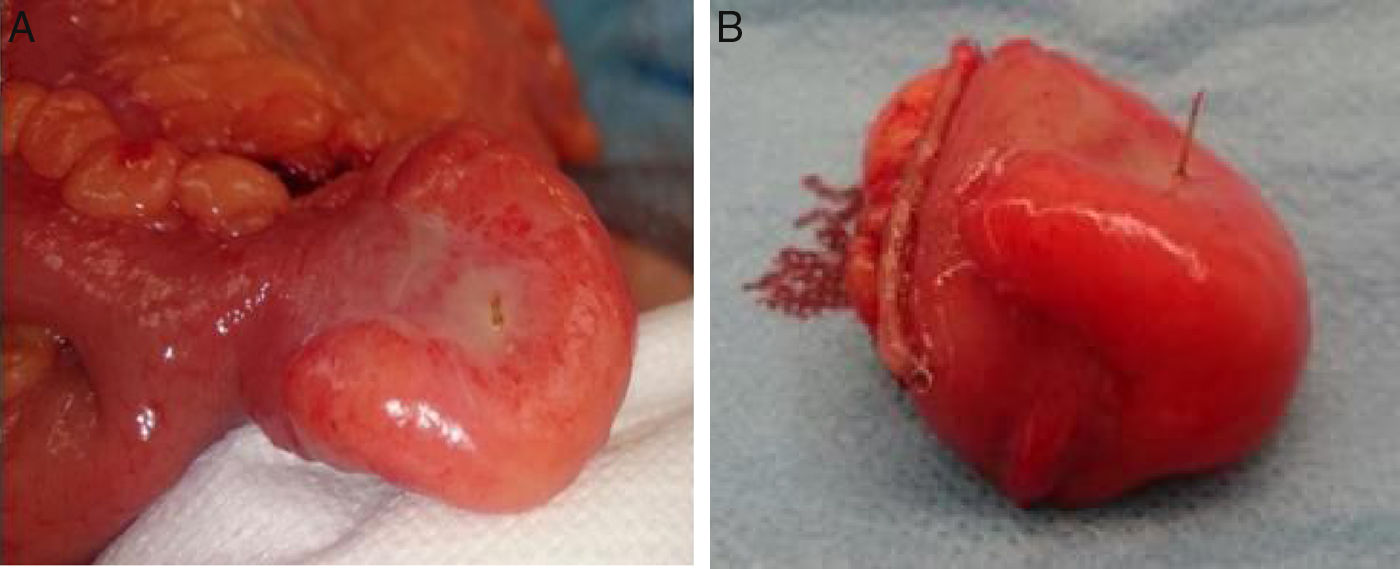
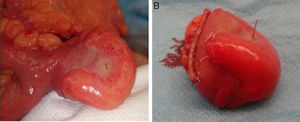
A 71-year-old man with a past medical history of COPD and peptic ulcer sought medical attention for abdominal pain in the right iliac fossa of 24-h progression, associated with hyporexia. There was no other accompanying symptomatology. Physical examination revealed pain in the lower hemiabdomen with guarding, as well as the Blumberg's sign and Rovsing's sign. Laboratory results reported leukocytosis (11,280/μl) with 63.3% segmented neutrophils and a slightly increased C-reactive protein level (1.2mg/dl). Clinical diagnosis of acute appendicitis was made, indicating urgent surgery. A cecal appendix with normal characteristics was observed through a pararectal incision, and so the small bowel was explored. An 80-cm MD of the ileocecal valve was identified, with inflammatory signs secondary to perforation by a foreign body, suggestive of a fish bone, with fragments of fibrin in the surrounding area (fig. 1A). Appendectomy was performed along with a Meckel diverticulectomy, sectioning its base with a linear stapler (fig. 1B). The histopathologic study confirmed the normality of the vermiform appendix, as well as the inflammatory changes in the MD. The patient had favorable postoperative progression and was released on day 6 after the surgery. He was asymptomatic at month 6 of follow-up.
MD is generally asymptomatic and only 4.2-16.9% have clinical manifestations.3 It is usually an incidental finding, identified in imaging studies or interventions performed for a different indication. When symptoms do present, they tend to be similar to those of acute appendicitis or those derived from a complicated MD. Bowel obstruction (35%), gastrointestinal bleeding (32%), diverticulitis (22%), umbilical fistula (10%), or perforation secondary to a foreign body (5%) are among the possible complications.4 The differential diagnosis for MD should include acute appendicitis, peptic ulcer, gastroenteritis, biliary colic, and colonic diverticulitis.5
Plain abdominal x-ray, ultrasound, and computed tomography are complementary studies, and even though they are not very specific, they can aid in the differential diagnosis of acute abdomen. They are also useful in cases in which the MD presents as an obstruction or perforation.5 Tc-99m scintigraphy has high sensitivity and specificity, but the number of false positives and false negatives increases with patient age, most likely due to technical difficulty and the overlap of the gallbladder over the area of the MD.5 Thus, it is not a study that is routinely used, but it is considered the technique of choice in cases of lower gastrointestinal bleeding in children suspected of having a MD.
Management of asymptomatic MD is controversial. According to a review from the Mayo Clinic on patients seen within the time frame of 1950 and 2002, prophylactic resection is not recommended, except in cases presenting in males under 50 years of age, with a MD that is longer than 2cm or has heterotopic tissue.6 However, in a study by Cullen et al., they recommend prophylactic resection in all patients under 80 years of age, considering that 6.4% of patients with MD can develop complications.7 In contrast, there is agreement that all symptomatic MDs should be surgically treated. The most widely used techniques are diverticulectomy and bowel resection. Diverticulectomy is the method of choice, as long as complete extirpation is certain, or the perforation is far from the base. It can be performed through wedge resection or with linear staplers. Bowel resection is indicated in cases of bleeding, diverticulitis, perforation close to the base, tumor, and in wide-based MDs or those in which wedge resection involves an intraluminal stricture.8,9 Minimally invasive techniques, such as laparoscopy, should be considered. It is a safe diagnostic procedure, as well as a therapeutic tool, reducing diagnostic delay, and consequently, morbidity and mortality, while keeping costs at a minimum.9
Diagnostic delay in a case of symptomatic MD can reach a 6% mortality rate, especially in the elderly.3 Therefore, it is necessary to be aware of this entity when making the differential diagnosis for acute abdomen, especially in patients with symptoms consistent with acute appendicitis. When acute appendicitis is not confirmed, the final 180cm of the small bowel should be examined, searching for a possible complicated MD and proceeding with its correct treatment.5
Authorship/collaborationsMarta Merayo-Álvarez worked in data acquisition and collection, and in the writing of the article. Daniel Fernández-Martínez participated in data acquisition and collection, and in the writing of the article and its critical review. Jessica Gonzales-Stuva participated in data acquisition and collection, and in the writing of the article. Lourdes Sanz-Álvarez participated in data acquisition and collection, and in the writing of the article. José Antonio Álvarez-Pérez carried out a critical review and the final approval of the article.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Merayo-Álvarez M, Fernández-Martínez D, Gonzales-Stuva J, Sanz-Álvarez L, Álvarez-Pérez JA. Perforación de divertículo de Meckel por cuerpo extraño. Revista de Gastroenterología de México. 2019;84:112–114.