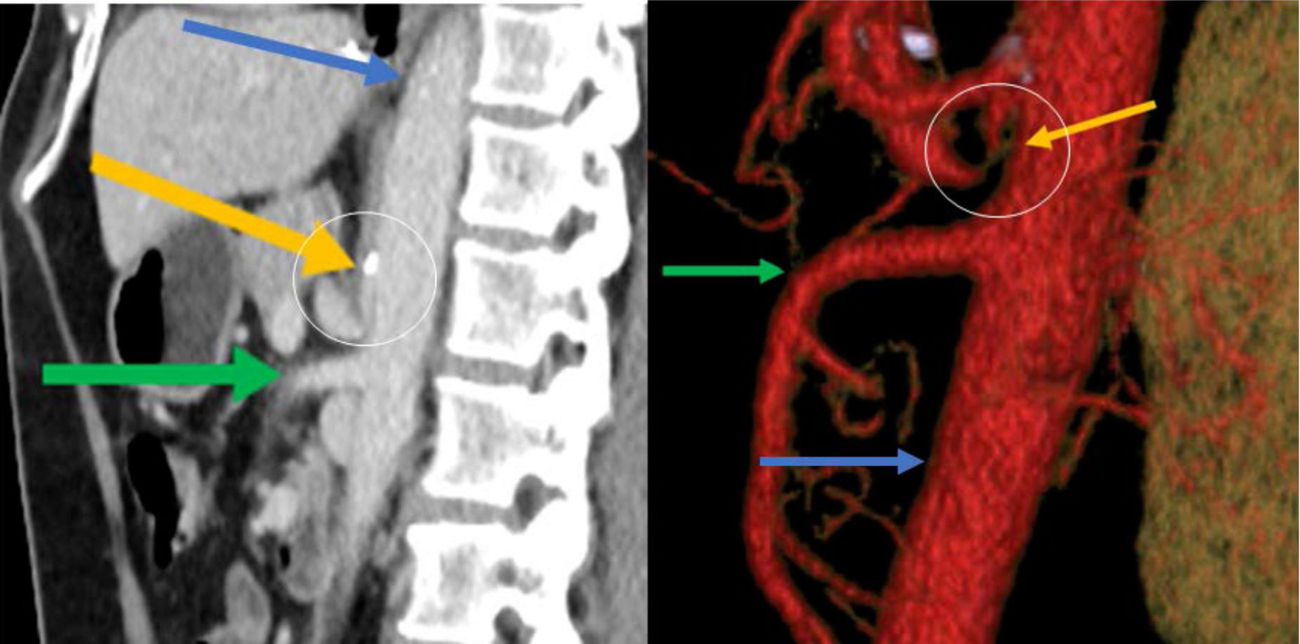
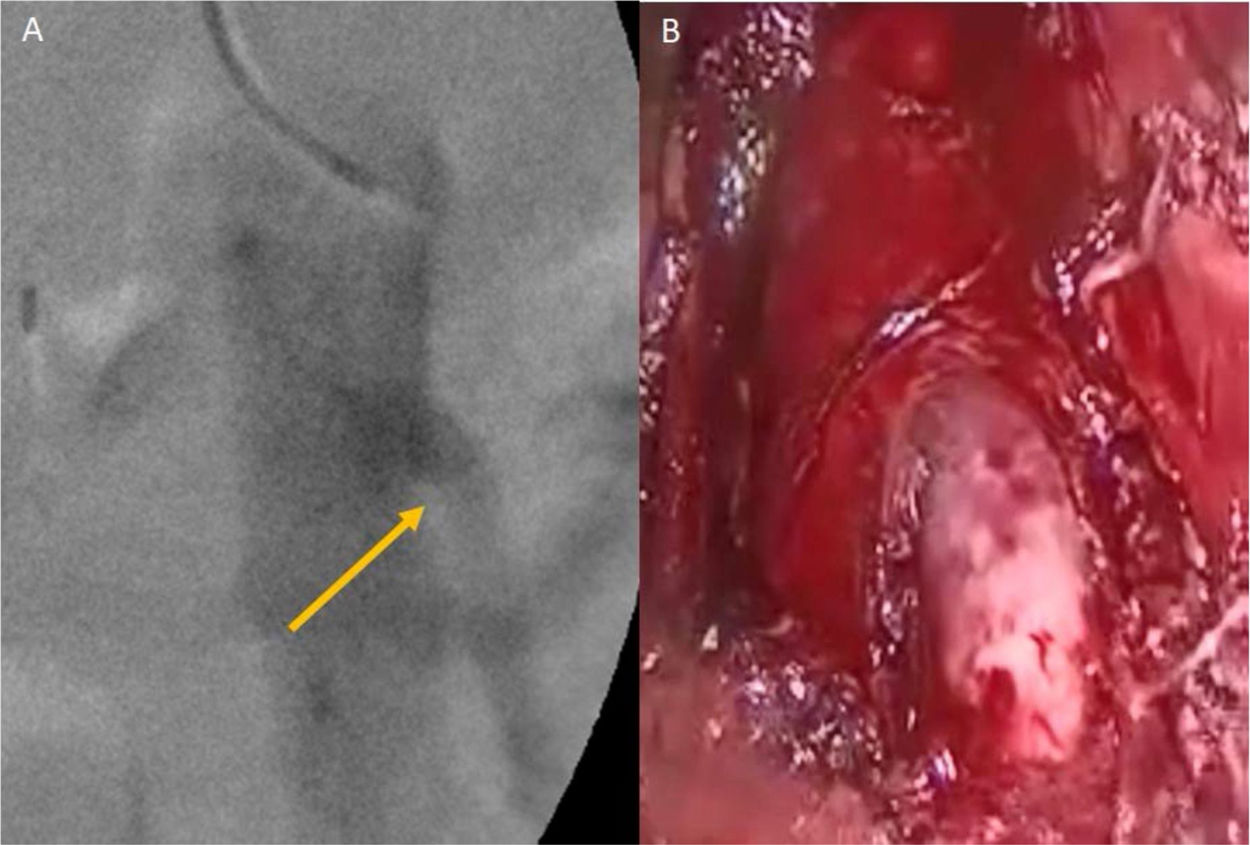
A 66-year-old man had a surgical history of laparoscopic fundoplication in 1995 and laparoscopic cholecystectomy in 1996. He arrived at the emergency department due to predominantly moderate, sharp, pulsating pain in the epigastrium that was associated with food intake, and to nausea, vomiting, change in bowel movement pattern, and general malaise. The patient stated he had presented with the same pain over a 20-year period, for which he was studied on numerous occasions by different gastroenterologists, undergoing endoscopy procedures and tomography exams (the latest two years prior) but not resulting in an accurate diagnosis. Physical examination showed normal vital signs and a murmur in the epigastric region, with no signs of peritoneal irritation. A contrast-enhanced computed tomography angiogram identified a reduction in the caliber of the origin of the short segment of the celiac trunk, with upward angulation of almost the entire celiac trunk, caused by the median arcuate ligament (Fig. 1A and B). A Doppler ultrasound was then carried out that showed a systolic velocity of 582cm/s during expiration (normal value: below 350cm/s), as well as a difference in the flow velocity during inspiration. Endovascular cannulation of the celiac trunk through the humeral artery was initially performed by the vascular surgery service, identifying important angulation of the celiac trunk (Fig. 2A). Afterwards, a laparoscopic procedure was performed at the general surgery service, finding fibrosis and adhesions at the level of the pillars of the diaphragm. Dissection was carried out until the celiac trunk was identified, which was found to be extrinsically compressed by the median arcuate ligament (Fig. 2B). The celiac trunk was freed, revealing its trifurcation, and its correct release from compression and flow improvement were corroborated by angiography. The patient was discharged on the second postoperative day, tolerating oral diet, experiencing no pain, and with 50% symptom improvement. At postoperative follow-up at one month, 2 months, and 9 months, the patient had 100% symptom improvement, stating that he was asymptomatic.
Sagittal reconstruction of the abdominal CT angiogram in the arterial phase, showing a reduction in the caliber of the origin of the short segment of the celiac trunk, with its upward angulation. The yellow arrow indicates the celiac trunk, the green arrow the superior mesenteric artery, and the blue arrow the aorta. The angulation of the celiac trunk can be seen inside the circle at the level of the calcification. A) Sagittal view, B) Reconstruction.
The present case illustrates a rare cause of chronic abdominal pain, and few such cases have been reported in the Spanish language literature. Albrecht von Haller described the celiac trunk in 1740, and since then, there have been important changes in the understanding of surgical anatomy and upper gastrointestinal irrigation. It was not until 1965 that David Dunbar, in his 15-patient case series, described the involvement of the celiac trunk in chronic epigastric abdominal pain of uncertain diagnosis.1 The median arcuate ligament (MAL) is formed by the thickened aponeurosis of the psoas muscle and is a product of the fusion of the tendons of the diaphragmatic crura. It extends from the L1 transverse apophysis to the L2 vertebral body.2 The diagnosis of median arcuate ligament syndrome (MALS), or Dunbar syndrome, requires great clinical suspicion because its symptoms are nonspecific and it is commonly confused with biliary disease, gastroesophageal reflux disease (GERD), chronic pancreatitis, and mesenteric ischemia.3 Its clinical presentation in 80-95% of cases is chronic abdominal pain, when lying down, that increases upon exhalation; unintentional weight loss in 50% of cases; and epigastric murmur, which is very suggestive of the disease, in 35% of cases.4,5 Our patient complained of intermittent epigastric pain, and arriving at the accurate diagnosis was a challenge for the clinicians. The systolic murmur was the sign that led to the correct diagnosis. Contrast-enhanced tomography is utilized when there is diagnostic suspicion and the definitive diagnosis is made through Doppler ultrasound, during inspiration and expiration. A systolic velocity above 350cm/s upon expiration, or a difference greater than 200cm/s, is diagnostic. Angiography is considered the diagnostic standard.6 Our patient had a flow > 500cm/s, confirming the MALS diagnosis. Treatment is based on division of the MAL and the celiac plexus fibers, with immediate improvement in 96% of cases and a 5-10% recurrence rate. Management with an endovascular stent has been shown to be useful in up to 75% of cases of recurrence.7
Di Libero et al.8 described the case of a patient with GERD and MALS, who underwent fundoplication and MAL release. To the best of our knowledge, the only association of MALS following a fundoplication is that reported by Ferreira et al.,9 involving a 53-year-old woman. Our hypothesis is that surgical manipulation can induce angulation and stricture. That association is barely mentioned in the literature, despite the etiologic similarity.
Finally, it is important to emphasize the complete symptom response to surgical treatment. In cases of chronic abdominal pain, in which common diseases of the gastrointestinal tract have been ruled out, syndromes such as MALS should be specifically looked for. Because it is a rare syndrome, diagnosis is a challenge for the physician, and once it is defined, surgical treatment generally results in 100% resolution of symptomatology.
Ethical considerationsThe authors declare that no experiments were conducted on humans or animals for the present study and that they have followed the protocols of their work center on the publication of patient data, preserving patient anonymity at all times.
The authors declare they have received the informed consent from the patient described in the article.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Zambrano-Lara M, Gonzalez-Urquijo M, Lozano-Balderas G, Rodarte-Shade M, Fabiani MA. Síndrome de ligamento arcuato medio como causa poco frecuente de dolor abdominal crónico. Revista de Gastroenterología de México. 2021;86:199–201.