Gastrointestinal infection due to cytomegalovirus (CMV) in patients with HIV has not been frequently reported. Its main presentation is perforation at the level of the colon, ileum, and appendix.1 Therefore, the aim of this work was to present a case of intestinal perforation at the level of the jejunum due to CMV during antiretroviral treatment (ART), as part of immune reconstitution inflammatory syndrome (IRIS).
A 48-year-old man had a past medical history of HIV infection. At the time of diagnosis, he presented with a viral load of 100,000 copies with a count of 47 CD4+ cells, signifying stage C3 disease.
The patient’s illness began in November 2021. He presented with asthenia, adynamia, and a productive cough that caused vomiting and dyspnea, but no cyanosis. Symptomatology had persisted for 21 days. He also had dyspnea after small and medium exertion and polypnea. Fourteen days after symptom onset, he presented with blood in sputum and a rise in body temperature accompanied by chills, piloerection, and diaphoresis, for which he sought medical attention at the emergency service of our hospital. The patient was evaluated and admitted to the internal medicine service on November 11, 2021, diagnosed with pneumonia in an immunocompromised patient. ART was started with tenofovir/emtricitabine (1 tablet of lopinavir/ritonavir every 24hours and 2 tablets every 12hours, together with trimethoprim-sulfamethoxazole and ceftriaxone). About two weeks after starting treatment, the patient began to have colicky abdominal pain located in the left iliac fossa, with intermittent intensity of 7/10, accompanied by nausea but no vomiting. Physical examination revealed abdominal pain and a soft abdomen upon palpation, rebound tenderness, and abdominal wall rigidity. A chest x-ray showed subdiaphragmatic free air. Pneumoperitoneum was identified in the supramesocolic recesses, predominantly in the right subdiaphragmatic region, with data of intestinal obstruction due to dilation of the stomach. He also presented with segments of the small intestine measuring up to 49mm and intestinal pneumatosis, and a transition zone at the level of the distal ileum was observed.
The laboratory work-up reported leukocytes 7.1×103/μL, hemoglobin 12.4g/dL, hematocrit 36.7%, platelets 445.0×103/μL, neutrophils 95%, absolute neutrophils 6.7×103/μL, lymphocytes 4.3%, absolute lymphocytes 0.31, CD4 0.68%, and absolute CD4 6.10 cells/μL.
The patient was taken to the operating room, where 100mL of intestinal fluid was drained, and perforation at the level of the jejunum, 60cm from the angle of Treitz in 30% of its lumen, was identified. Friable circular lesions also occupied 20% of the intestinal lumen at 100cm from the angle of Treitz (Fig. 1). Primary closure was carried out with PDS 4.0 on two planes and samples of the edges of the intestinal perforation were sent to the pathology service of the hospital.
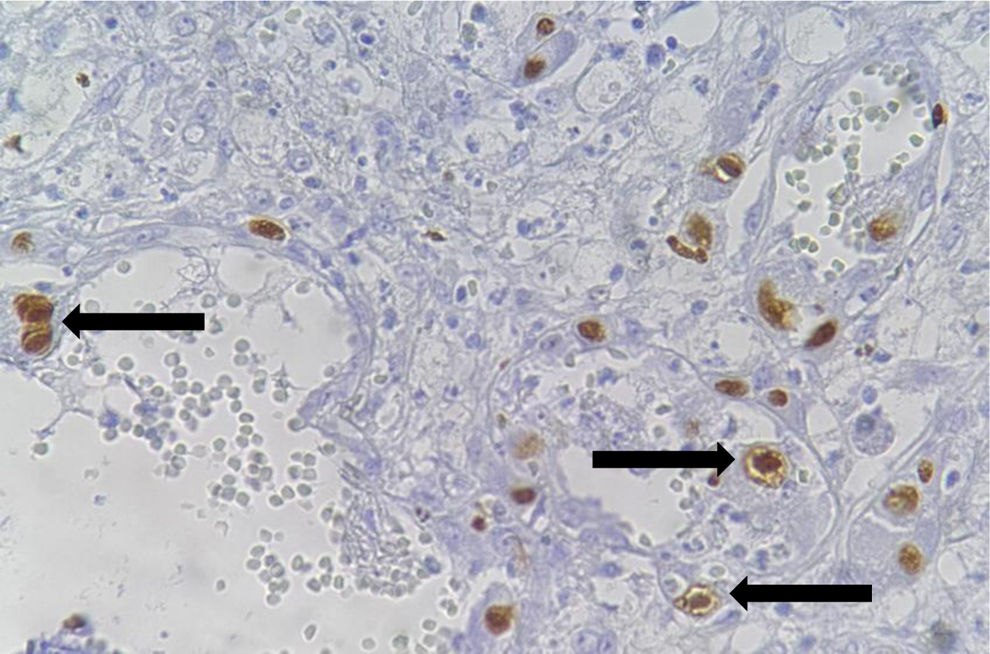
The pathologic analysis identified an extensive cytopathic effect in endothelial cells and macrophages, characteristic of CMV infection that was confirmed through immunohistochemistry and a PCR test (Fig. 2). Treatment was started with ganciclovir for 14 days. The patient had adequate clinical progression and was released in 30 days.
Intestinal perforations due to IRIS associated with CMV infection are not often reported. It affects immunodepressed patients, particularly those with CD4 levels below 50 cells/mm3, which can cause ulceration, enterocolitis, ischemia, and perforation.2–7 To the best of our knowledge, the case presented herein is the first to be reported in Mexico. At the time of this writing, only three cases of perforation at the level of the jejunum, including this one, have been reported.4,5
The most common symptomatology in this kind of disease is fever, abdominal pain, and diarrhea, and its presentation can sometimes be asymptomatic. Our patient also presented with pneumonia, further compromising his recovery. Nevertheless, he improved with the treatment with ganciclovir for 14 days, and so was released from our hospital.
The pathogenesis caused by CMV is believed to occur due to submucosal vasculitis in conjunction with thrombosis, resulting in ischemia, ulcers, and intestinal wall thinning, which can cause its later perforation and gangrene.8 Thus, CMV-induced gastrointestinal perforation together with IRIS can be considered, especially in persons with HIV infection during ART.3
As part of the treatment of our patient, we decided on primary closure of the lesion due to its size and closeness to the angle of Treitz. The patient’s postoperative progression during the three months of follow-up was favorable.
It is important to consider IRIS as a cause of the complication of acute abdomen in patients with AIDS, after starting antiretroviral therapy, especially in those with a very low baseline CD4 count. Therefore, starting ART early and maintaining a high CD4+ T cell count is necessary.
Ethical considerationsThe authors declare that this case report contains no personal information that can identify the patient, and so informed consent was not required. Nevertheless, informed consent was obtained for the publication of the present work. In addition, this case report meets the current bioethics research regulations and did not need to be authorized by the institutional ethics committee because it did not affect the patient’s health.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this article.
Author contributionsAll authors have read the manuscript and agree with the version to be published.
Conflict of interestThe authors declare that there is no conflict of interest.
The authors wish to thank Dr. Guillermo Manuel González Müller, who made the histopathologic diagnosis.