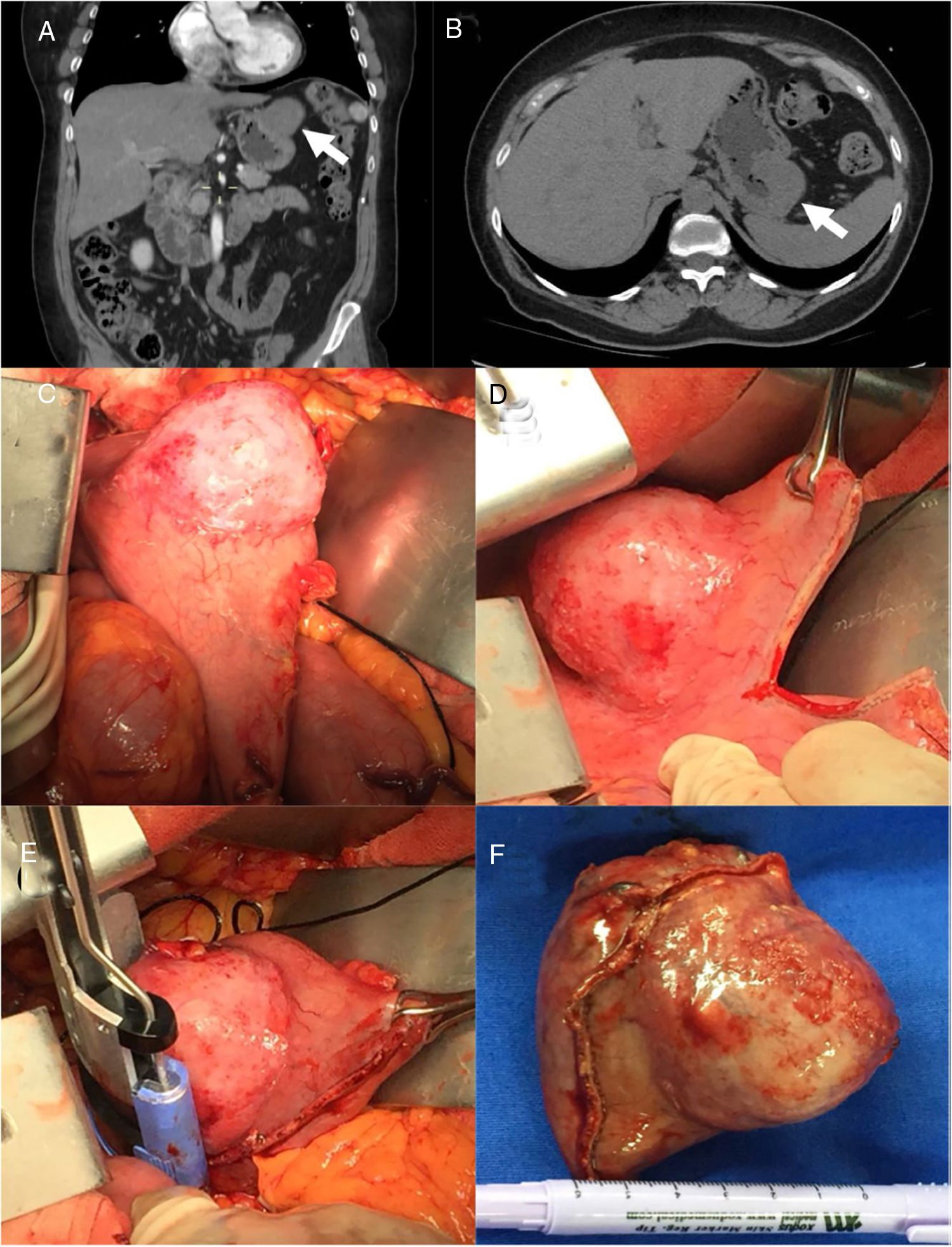
A previously healthy 55-year-old woman sought medical attention at our department complaining of epigastric pain of 6-month progression, accompanied by heartburn and early satiety. She had been taking over-the-counter proton pump inhibitors and prokinetics, with no clinical improvement. We scheduled her for an abdominal computed tomography scan and upper endoscopy. However, before her appointment, she presented with an episode of melena and went to the emergency department, at which time the abovementioned studies were then carried out. Endoscopy revealed a submucosal growth over the anterior portion of the gastric fundus, with no signs of active bleeding. Following stabilization, a computed tomography scan of the abdomen and pelvis was ordered, identifying an exophytic, well-defined (4.4 × 5.2 cm) tumor over the gastric fundus, with no signs of locally advanced or metastatic disease (Fig. 1A and B). An endoscopic ultrasound study confirmed lesion invasion through the muscularis propria, precluding the safe performance of endoscopic resection. The patient was then scheduled for surgery the following day.
Abdominal computed tomography scan with coronal (A) and sagittal (B) views, showing focal thickening of the gastric fundus and an exophytic (4.4 × 5.2 cm) lesion with well-defined borders (white arrows). Neoplastic lesion of the anterior gastric fundus (C). Surgical images displaying wedge resection performed with a combination of linear (D) and curved (E) staplers. Surgical specimen after successful resection, measuring 7 × 5 cm (F).
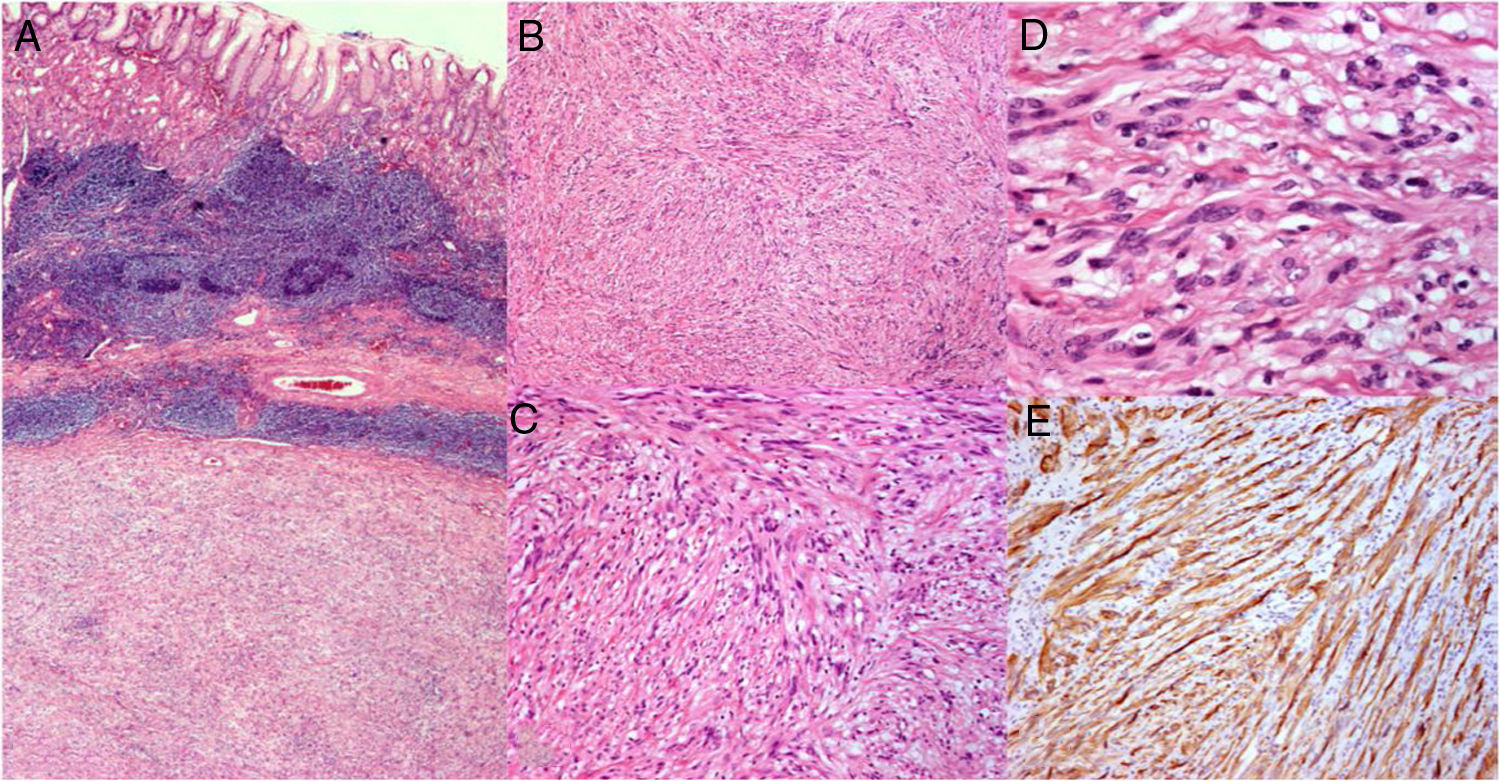
During the surgical procedure, a supraumbilical midline incision was made, followed by an extensive wedge resection of the stomach that enabled complete tumor extraction (Fig. 1D and E). A 7 × 5 cm specimen was obtained, and no peritoneal implants, adenopathies, or metastases were found. The histopathologic analysis reported a gastric schwannoma (GS) with negative margins and a mitotic index of 1/50 high power fields (Fig. 2). The patient was discharged after an uneventful postoperative period and has been followed at our outpatient clinic. At present, she shows no signs of recurrence or morbidity.
A section of the surgical specimen (×40) (A). A well-circumscribed submucosal mesenchymal tumor arising from the sheath of Auerbach’s plexus, consisting of spindle cells arranged in cross bundles accompanied by hyalinized fibrillar material (B, C, D). Immunohistochemistry displaying S-100 and glial fibrillary acidic protein positivity (E).
GSs are benign, mesenchymal, slow-growing tumors that originate from Schwann cells. They account for 6.3% of all gastric mesenchymal tumors and 4% of all benign gastric tumors. When schwannomas are found in the gastrointestinal tract, they usually arise from the nerve sheath of Auerbach’s plexus. Female predominance has been described in the literature, with a male:female ratio of 1:3 and an average age at diagnosis of 57 years. Patients with GS are usually asymptomatic, and the tumor is an incidental finding in 43.3% of cases. Symptomatic patients typically present with abdominal pain, followed by upper gastrointestinal bleeding. Less frequently, they present with a palpable abdominal tumor (3%), anorexia (3%), dyspepsia (1.8%), weight loss (1.2%), and vomiting (0.6).1
Preoperative work-up can be misleading in patients with GS. Computed tomography usually reveals a well-circumscribed lesion, but radiologic findings are not very specific and are often suggestive of a gastrointestinal stromal tumor. Upper gastrointestinal endoscopy shows GSs as solid submucosal sessile tumors that frequently have an ulcerated mucosa, whereas endoscopic ultrasound identifies a hypoechoic lesion arising from the fourth echo layer of the stomach. Endoscopic ultrasound enables the performance of fine needle aspiration biopsy during the procedure, which is diagnostic in up to 85.2% of cases.2 Histopathologic analysis is the current gold standard of diagnosis. Schwann cells are characteristically arranged in a fascicular manner and display positive immunohistochemistry for protein S-100, vimentin, and glial fibrillary acidic protein, confirming the diagnosis.3 Surgical resection is the only curative treatment for GS, and the specific type of procedure will depend on the size and location of the lesion. Endoscopic resection is not feasible in most cases, because the neoplasia usually arises from Auerbach’s plexus, and growths tend to involve the entire width of the muscularis propria. On the other hand, minimally invasive (laparoscopic) techniques have shown satisfactory results. Formal lymph node resection is not necessary, as GSs seldom have lymphatic dissemination or malignant transformation. Only a few such cases have been reported in the medical literature.
Financial disclosureNo financial support was received in relation to the present article.
Conflict of interestThe authors declare that there are no conflicts of interest.
Ethical considerationsThe authors declare that informed consent was signed by the patient for publication of the present manuscript, which abides by our institutional ethics committee policies and norms. The authors also declare that the present article contains no identifying personal information of the patient.
Please cite this article as: Sánchez-Morales GE, et al. Schwannoma gástrico: una rareza entre los tumores mesenquimatosos del tracto gastrointestinal. Revista de Gastroenterología de México. 2020;85:102–104.