Helicobacter pylori (Hp) infection is one of the most common infections in humans. Due to its worldwide prevalence, a series of guidelines and recommendations has been developed for the appropriate screening, diagnosis, and management of patients with Hp infection.
AimTo evaluate the approach, attitudes, and knowledge of a group of Mexican general practitioners in relation to Hp.
Materials and methodsA cross-sectional study was conducted that evaluated the knowledge of Hp diagnosis and treatment through the application of a questionnaire.
ResultsFrom the total of 430 questionnaires delivered, information was obtained from 411 (95% response rate). The most frequent indications for eradication treatment were peptic ulcer (48.4%), gastroesophageal reflux disease (41.8%), and dyspepsia (39.2%). Thirty-one percent of the physicians surveyed used more than one test to look for Hp, and serology was the most commonly employed method. The most widely used antibiotic regimen was clarithromycin plus amoxicillin (63.8%), followed by metronidazole plus tetracycline (16%). Ninety-two percent of the physicians confirmed eradication through endoscopy for the histologic analysis and only 23% utilized the breath test.
ConclusionsOur results show the lack of knowledge about the established diagnostic and treatment recommendations for Hp infection. The implementation of workshops, courses, and conferences, or the formulation of practical guidelines should be directed at primary care physicians to strengthen the practice of medicine based on scientific evidence.
La infección por Helicobacter pylori (Hp) es una de las más comunes en el humano. Debido a su alta prevalencia a nivel mundial se ha desarrollado una serie de guías y recomendaciones para el apropiado escrutinio, diagnóstico y manejo de los pacientes con Hp.
ObjetivoEvaluar el abordaje, las actitudes y el conocimiento acerca de Hp en un grupo de médicos generales en nuestro país.
Materiales y métodosEstudio transversal en el cual se evaluaron, mediante la aplicación de un cuestionario, los conocimientos acerca del diagnóstico y tratamiento de Hp.
ResultadosDe un total de 430 encuestas entregadas, se obtuvo información proveniente de 411 (tasa de respuesta del 95%). Las indicaciones más frecuentes de tratamiento de erradicación fueron la úlcera péptica (48.4%), la enfermedad por reflujo gastroesofágico (41.8%) y la dispepsia (39.2%). El 31% de los médicos utilizan más de una prueba para la búsqueda del Hp, de las que la serológica es la más utilizada. El esquema de antibióticos más utilizado es claritromicina más amoxicilina (63.8%), seguido de metronidazol más tetraciclina (16%). El 92% de los médicos corroboran la erradicación mediante una endoscopia para el análisis histológico y la prueba de aliento solo se utiliza en el 23%.
ConclusionesNuestros resultados muestran la carencia de conocimientos sobre las recomendaciones de diagnóstico y tratamiento establecidas en la infección por Hp. La implementación de talleres, cursos, conferencias o la elaboración de guías prácticas deben dirigirse a los médicos de primer contacto con la finalidad de fortalecer la práctica médica basada en la evidencia científica.
Helicobacter pylori (H. pylori) infection continues to be one of the most common infections in humans.1 Up to half of the world population can have gastric colonization of this bacterium (Gram-negative, microaerophilic). Its most virulent strains (CagA +) have been related to different gastroduodenal pathologies, such as chronic gastritis, peptic ulcer, type B gastric lymphoma (MALT), and the possibility of developing adenocarcinoma through chronic alterations, such as atrophy and metaplasia.2
The prevalence of H. pylori varies, depending on factors such as socioeconomic status, hygienic conditions, lack of potable water, and overcrowding. Therefore, its frequency is greater in developing countries (70 to 90%), compared with developed countries (30 to 50%), and the infection is acquired in early childhood.3 A report from the World Gastroenterology Organization in 20104 reported the worldwide prevalence of H. pylori infection, and it included Central American and South American countries. In Mexico, prevalence in children between the ages of 5 and 9 years was 43%, and it was 70-90% in adults. In Guatemala, prevalence in children from 5 to 10 years was 51%, and 65% in adults.4 Prevalence in Bolivia, Brazil, and Chile varied from 30 to 54% in children and adolescents, and from 70 to 90% in adults.4
In Mexico, a national survey on an open population (n = 11,605) that used serum antibody determination as the screening method found an overall frequency of 66%.5 Seropositivity rose in direct relation to age, with figures higher than 80% in subjects over 30 years of age.5
Due to the high prevalence of H. pylori worldwide, a series of guidelines and recommendations for the appropriate screening, diagnosis, and management of patients with H. pylori infection have been developed within the last few years. The most recent Maastricht V Consensus6 reaffirms previous recommendations that have been sustained over time, such as eradicating the bacterium in patients with H. pylori and peptic ulcer, or eradication therapy as first-line treatment for low-grade gastric lymphomas (MALTomas).6 With respect to diagnosis, the main noninvasive tests that can be used for the “search and treat” strategy are the labelled urease breath test or the monoclonal antibody-based stool antigen test (Level of evidence: 2a; Grade of recommendation: B).6
In Mexico, a consensus published in 2007 (Third Mexican Consensus on Helicobacter pylori) established the guidelines for making decisions concerning this situation in our country.7 Those guidelines and recommendations consider specific situations, such as the high prevalence of H. pylori, the high frequency of infection in certain groups, and the lack of resources at some healthcare facilities for conducting special tests, as well as the high resistance to antibiotics.7
An elevated prevalence of gastrointestinal diseases or symptoms (for example, dyspeptic symptoms) in populations where H. pylori infection is high, implies that a large number of subjects receive primary health care. Therefore, it is essential that primary care physicians have the appropriate knowledge for making adequate decisions and preventing incorrect practices that result in elevated costs and absolutely no health benefits for the population. Even though there are initiatives in other countries for educating primary care physicians with respect to the diagnosis and adequate management of this infection, the results of various surveys carried out in developing countries reveal confusion and discrepancies regarding the pathogenesis, diagnosis, and treatment of H. pylori.8–11 A Peruvian study showed that up to 60% of primary care physicians and 69% of internists used inappropriate regimens for eradicating H. pylori and that only 8% knew this infection was associated with MALT lymphomas.12
Despite the high prevalence of H. pylori in Mexico, there are no previous studies conducted on primary care physicians with respect to their knowledge and practice in relation to H. pylori infection. The aim of the present study was to evaluate the approach to, attitudes about, and knowledge of H. pylori infection in a group of general practitioners in Mexico.
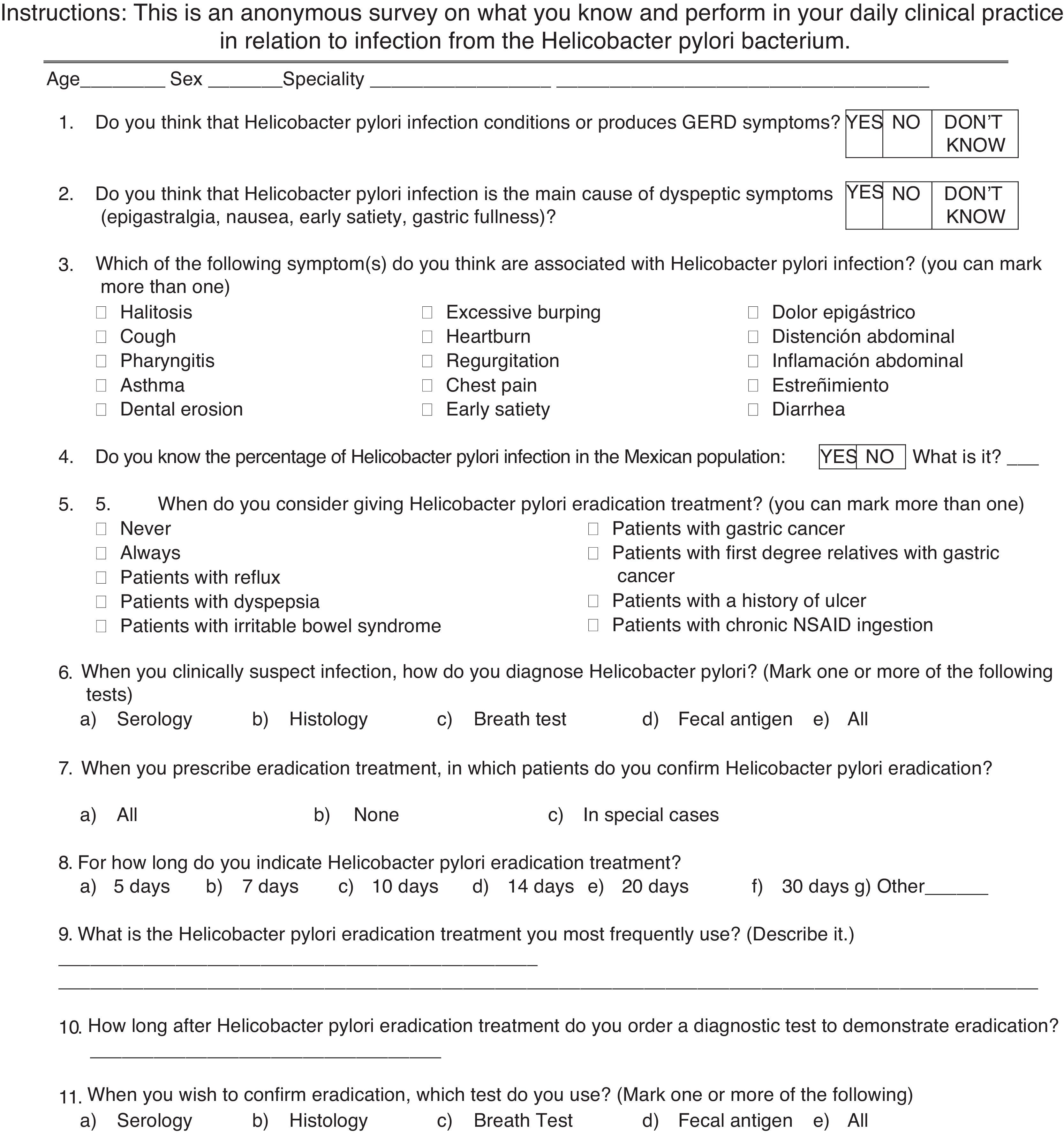
Materials and methodsA prolective and cross-sectional study was conducted through a questionnaire (11 questions, Annex 1) designed to evaluate the knowledge of the diagnosis and treatment of H. pylori on the part of general practitioners from the 32 States of the Mexican Republic that attended a training course (2 days, 8h each day) on gastrointestinal diseases, in groups of 30 to 40, at the Instituto de Investigaciones Médico Biológicas of the Universidad Veracruzana within the time frame of May 2013 and February 2015. All the questionnaires were answered anonymously, in blinded form, and voluntarily, before the commencement of the academic activities. Convenience sampling (non-probabilistic) was employed for the study. The Research and Ethics Committee of the Instituto de Investigaciones Médico Biológicas approved the work.
Descriptive statistics were carried out and the frequencies (95% confidence intervals) of the answers obtained for each question were calculated. The chi-square test and Student's t test, as appropriate, were used for the univariate analysis, and statistical significance was set at a p under 0.05. The multivariate analysis employed the ANOVA test and multinomial logistic regression. The statistical analysis was performed using the SPSS version 16 program (Chicago, Illinois, USA).
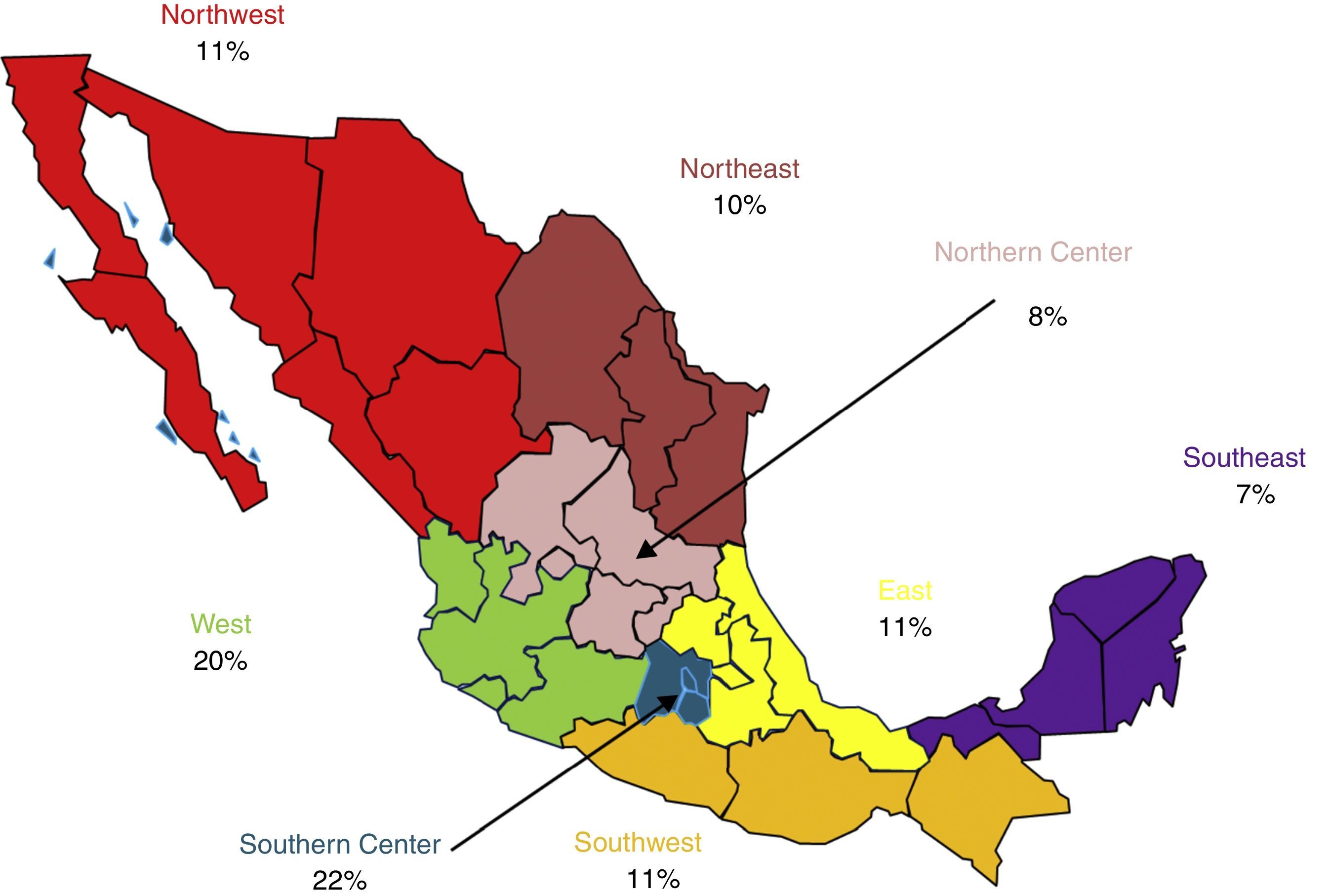
ResultsOf the total of 430 surveys given out, information was obtained from 411 (95% response rate). The total of 411 subjects evaluated consisted of 217 men (53%) and 194 women (47%), with a mean age of 50.9 ± 10.4 years (range: 23-78 years). The physicians had been practicing general medicine for a mean 5.7 years (range: 2-23 years) and saw a mean 14 patients (range: 8-22) per day. Figure 1 shows the percentage of physicians that came from the eight different geographic zones of Mexico.
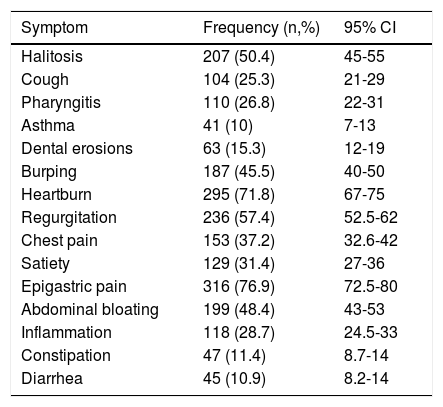
Of the total of the subjects evaluated, 339 (82.5%; CI, 78-85%) thought that H. pylori infection could cause gastrointestinal esophageal reflux disease (GERD) and 185 (45%; CI, 40%-49%) considered it the main cause of dyspepsia. The physicians thought that H. pylori caused GERD more frequently than dyspepsia (OR: 5.75; 95% CI: 4.17-7.92; p = 0.005). Table 1 shows a list of symptoms and the frequency with which the study group regarded them as the consequence of H. pylori infection. Only 21% (n = 88) of the physicians surveyed stated having knowledge of the estimated prevalence of H. pylori in Mexico and the mean of that estimated prevalence was 55.14% (range: 15-92%).
Symptoms that were considered caused by Helicobacter pylori infection.
| Symptom | Frequency (n,%) | 95% CI |
|---|---|---|
| Halitosis | 207 (50.4) | 45-55 |
| Cough | 104 (25.3) | 21-29 |
| Pharyngitis | 110 (26.8) | 22-31 |
| Asthma | 41 (10) | 7-13 |
| Dental erosions | 63 (15.3) | 12-19 |
| Burping | 187 (45.5) | 40-50 |
| Heartburn | 295 (71.8) | 67-75 |
| Regurgitation | 236 (57.4) | 52.5-62 |
| Chest pain | 153 (37.2) | 32.6-42 |
| Satiety | 129 (31.4) | 27-36 |
| Epigastric pain | 316 (76.9) | 72.5-80 |
| Abdominal bloating | 199 (48.4) | 43-53 |
| Inflammation | 118 (28.7) | 24.5-33 |
| Constipation | 47 (11.4) | 8.7-14 |
| Diarrhea | 45 (10.9) | 8.2-14 |
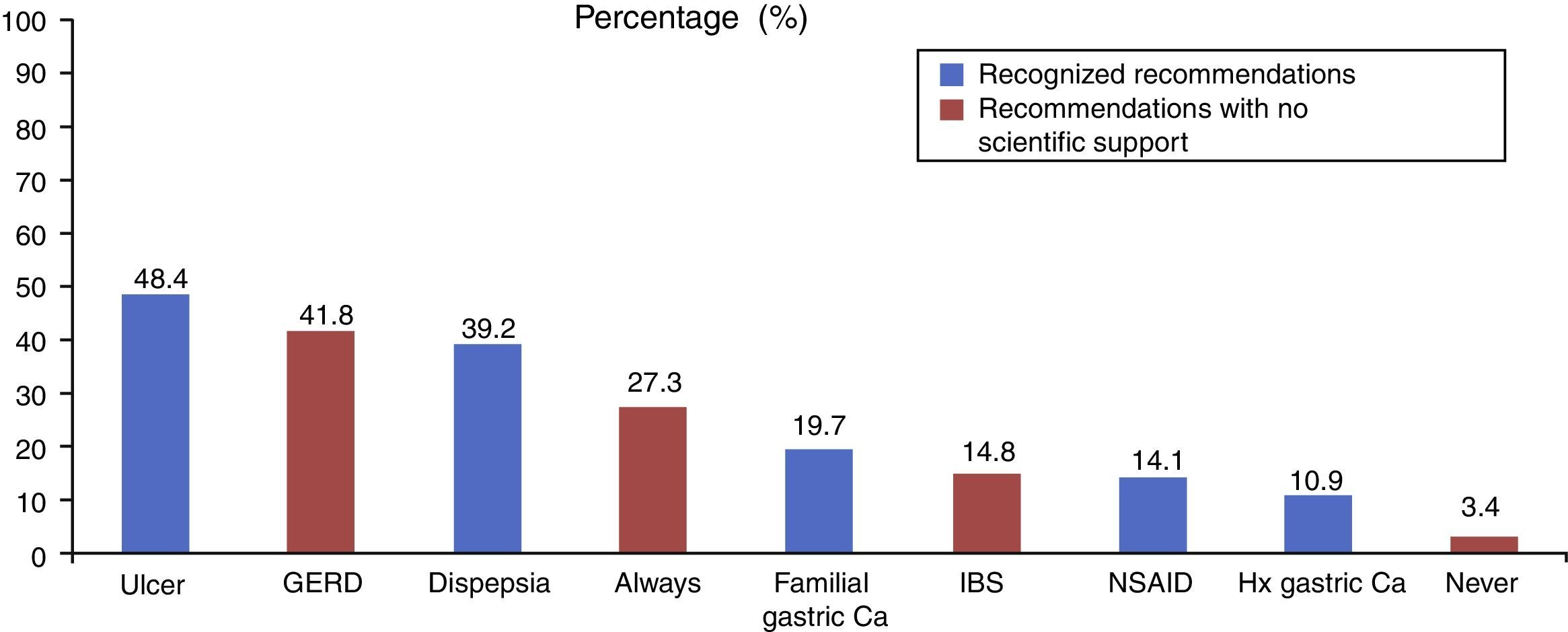
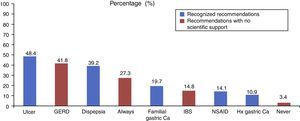
Figure 2 shows the most frequent indications for which the physicians prescribed H. pylori eradication treatment, based on accepted recommendations according to the Maastricht Consensus, as well as other recommendations with no scientific evidence.
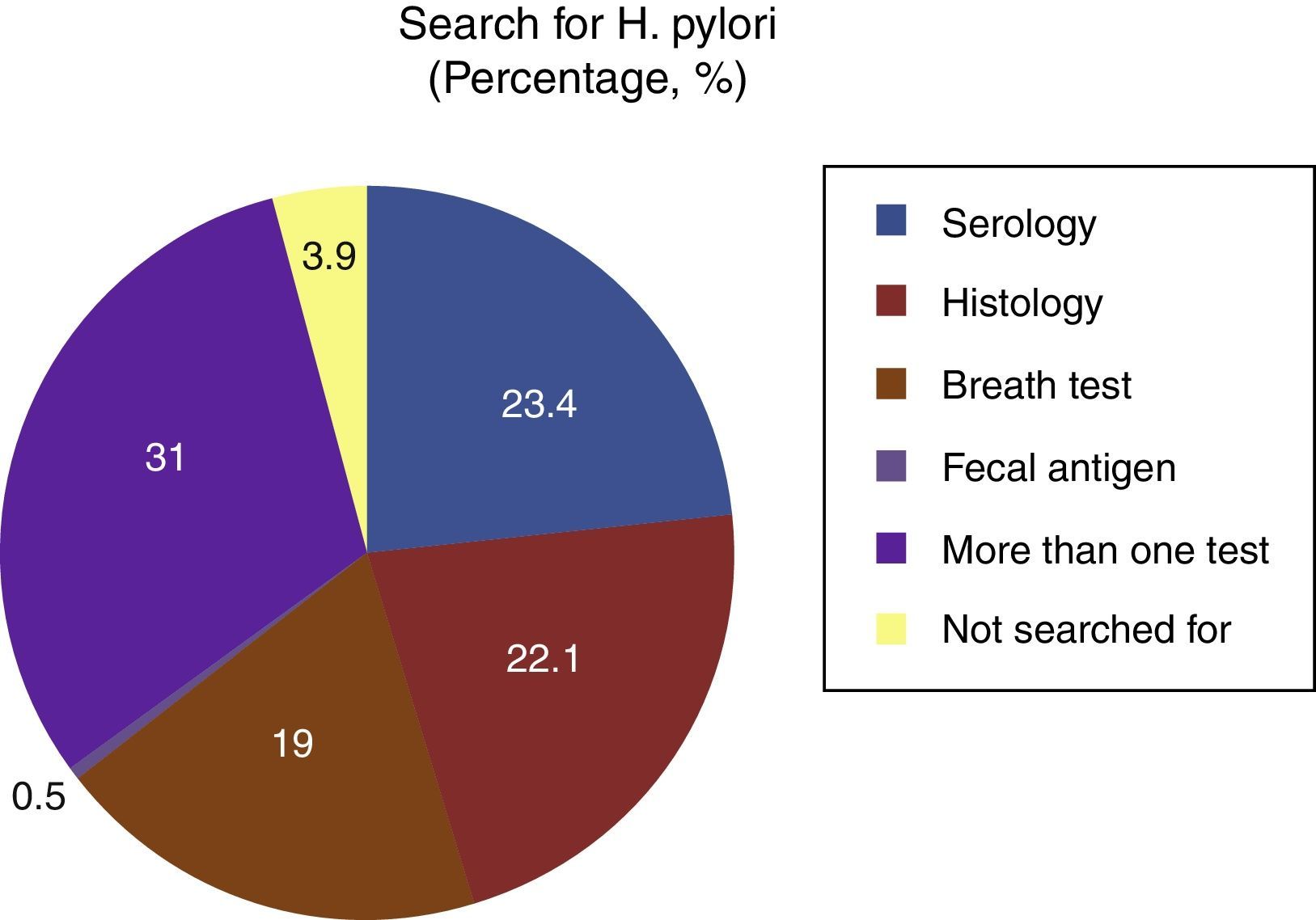
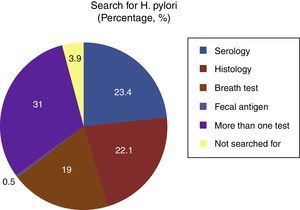
Figure 3 shows that the use of a single test (n = 127, 31%) was the most common for diagnosing H. pylori infection. Of those 127 physicians, 89% (n = 113) used 2 tests for making the diagnosis. The most frequent combination was serology + histology (77%), serology + breath test (18%), and histology + breath test (5%). Eleven percent (n = 14) stated that they used 3 tests, and the most common combination was serology + histology + breath test. When just one test was used, serology was the most common (23.4%). It was striking that the detection of fecal antigens in stool samples was hardly used (0.5%).
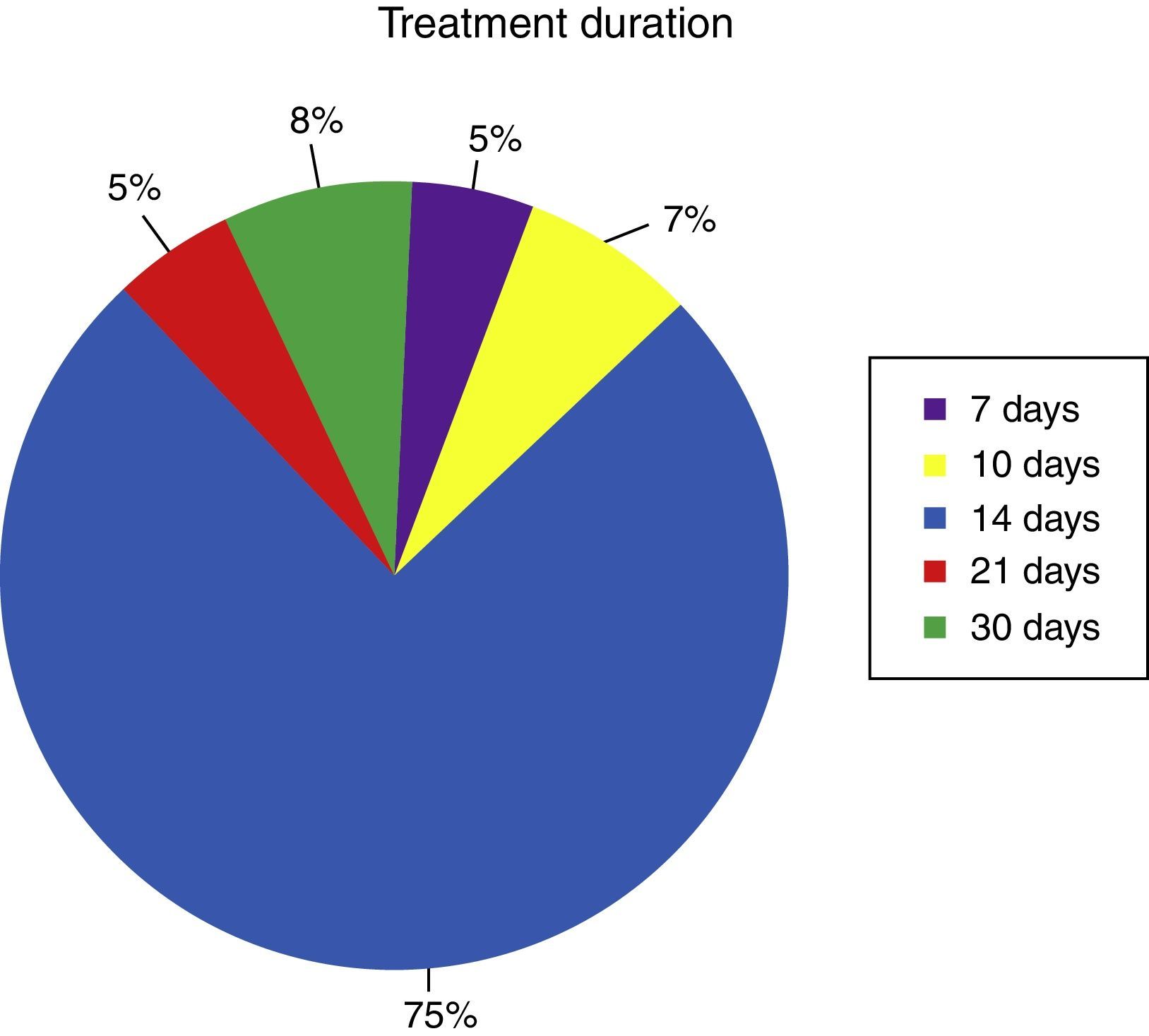
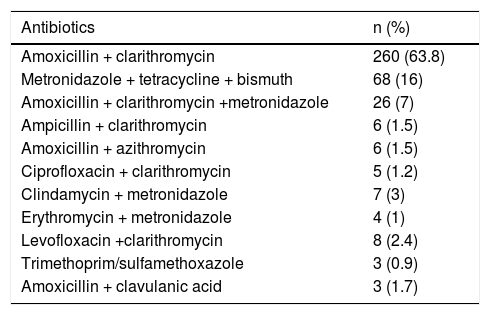
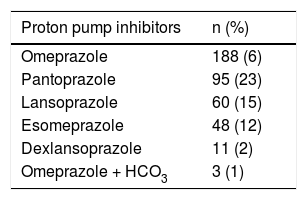
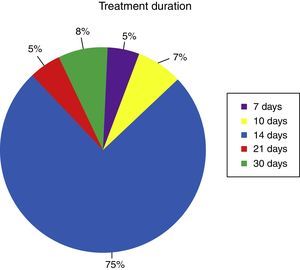
Table 2 shows the different antibiotic regimens used by the 397 subjects that indicated H. pylori eradication. The most widely used proton pump inhibitor (PPI) for the eradication scheme was omeprazole (46%), followed by pantoprazole (23%), and esomeprazole (15%) (Table 3). Figure 4 shows the duration of the prescribed treatment, and the most frequent (75%) was administration of the regimen employed for 14 days, followed by the uncommon recommendation of one-month regimens (8%).
Antimicrobial eradication regimens prescribed with greatest frequency.
| Antibiotics | n (%) |
|---|---|
| Amoxicillin + clarithromycin | 260 (63.8) |
| Metronidazole + tetracycline + bismuth | 68 (16) |
| Amoxicillin + clarithromycin +metronidazole | 26 (7) |
| Ampicillin + clarithromycin | 6 (1.5) |
| Amoxicillin + azithromycin | 6 (1.5) |
| Ciprofloxacin + clarithromycin | 5 (1.2) |
| Clindamycin + metronidazole | 7 (3) |
| Erythromycin + metronidazole | 4 (1) |
| Levofloxacin +clarithromycin | 8 (2.4) |
| Trimethoprim/sulfamethoxazole | 3 (0.9) |
| Amoxicillin + clavulanic acid | 3 (1.7) |
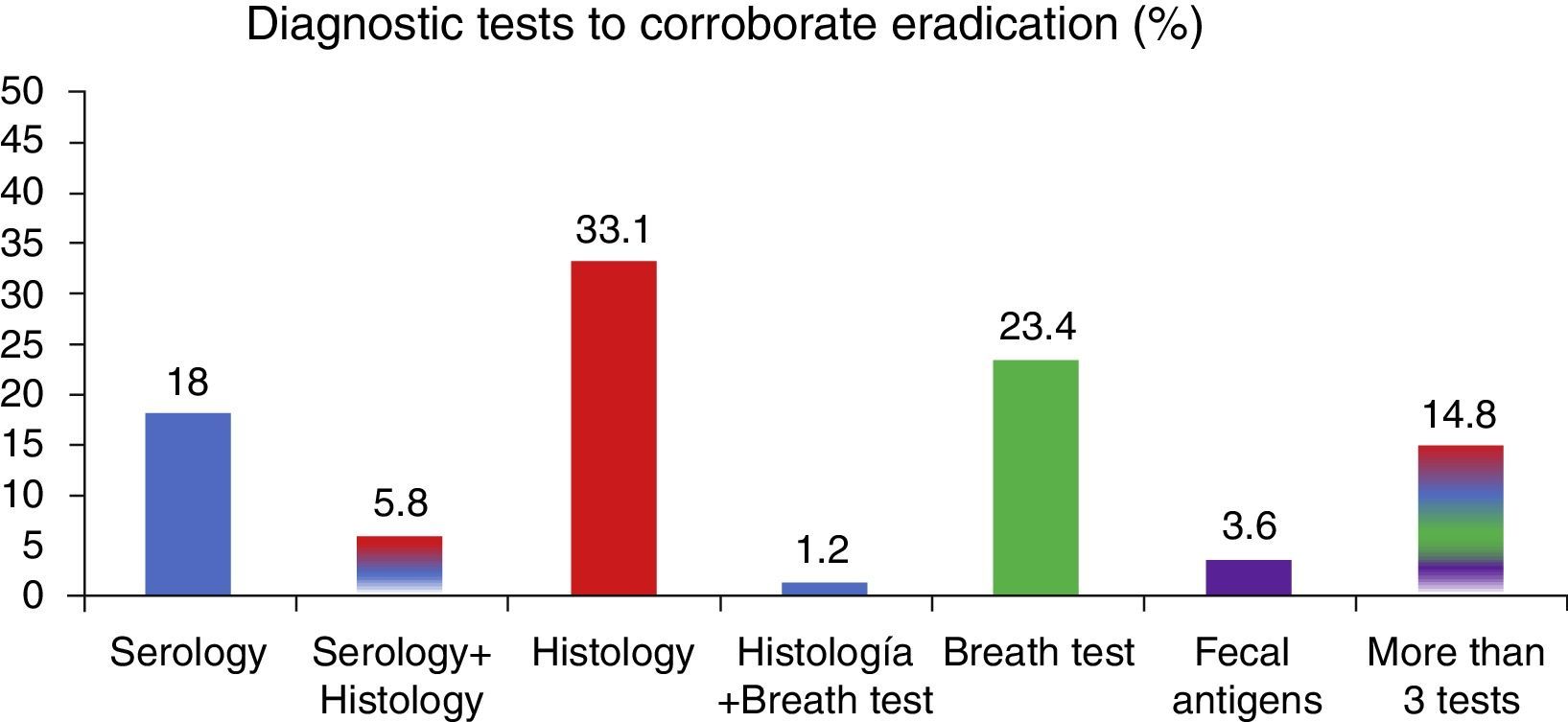
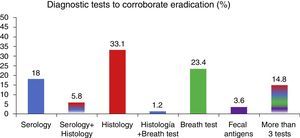
Ninety-two percent (n = 365) of the physicians corroborated the eradication of the bacterium after H. pylori eradication treatment and Figure 5 shows the methods utilized for its confirmation. It is surprising that the most common method for confirming eradication was a new endoscopy for histologic analysis and that the breath test was only used by 23% of the physicians. No statistically significant differences were found upon analyzing results according to the region the general practitioners were from, age, sex, or time practicing medicine (p > 0.05)
DiscussionH. pylori infection is frequent worldwide and the greatest number of cases are reported in developing countries. In Mexico, primary health care is handled by general practitioners or family physicians that have the first contact with patients. Thus, we paid special attention to this broad group, discovering important deficiencies in their knowledge, especially concerning the recommendations for the diagnosis and treatment of H. pylori infection. That information revealed an area of special interest for carrying out educational medical activities to improve primary health care.
The Maastricht V Consensus made recommendations about diagnostic strategies and treatment indications for H. pylori infection, considering it adequate to carry out intentional search and treatment in patients with uninvestigated dyspepsia, when there is high prevalence in the population (>20%). This is still a subject of debate in the Mexican environment, in which rates above 70% in the adult population have been reported, without taking patients with alarm symptoms into account (Level of evidence: 1a; Grade of recommendation: A). In a study involving 509 primary care physicians, Ahmed et al.13 reported the presence of dyspepsia symptoms (67%) as the main indication for performing a diagnostic test, followed by GERD, gastric or duodenal ulcer, and iron deficiency anemia.
In our study, dyspepsia was not the most common cause for contemplating H. pylori eradication. On the other hand, it should be mentioned that no evidence justifying the intentional search for H. pylori has been reported in patients with GERD, given that it has been demonstrated that there is no relation to symptoms, recurrence, and efficacy of treatment and its eradication does not exacerbate symptomatology (Level of evidence: 1a; Grade of recommendation: A). However, in our study, 82% of the participants considered that H. pylori was a cause of GERD symptoms.6 This situation is peculiar and inappropriate and most certainly results in many patients unnecessarily receiving eradication treatment in Mexico.
Upon analyzing the symptoms that the general practitioners frequently related to H. pylori infection, it was obvious that they associated this bacterium with symptoms for which there is no causal relation, such as halitosis (50%) or abdominal bloating (48%). The fact that only 21% of the participants believed they had knowledge of the prevalence of this infection in Mexico should also be underlined. Even more alarming was how the range of the presumed knowledge went from H. pylori being considered a low prevalence infection (15%) to a very high prevalence infection (92%). Such epidemiologic knowledge is essential, given that many of the diagnostic and therapeutic decisions made should be based on the true prevalence of the disease.
Among the main noninvasive diagnostic studies are the urea breath test and the monoclonal antibody-based stool antigen test (Level of evidence: 2a; Grade of recommendation: B). However, our study showed that the most widely used noninvasive test was serology, likewise reported by Ahmed et al., 14 Canbaz et al., 13 and Ghanaei et al.,11 reflecting the lack of adherence to the diagnostic recommendations. It is well known that serology is not useful for diagnosing active infection, much less for corroborating eradication, and its current usefulness is limited to epidemiologic studies. In fact, the most recent Maastricht V/Florence Consensus states that even though serologic tests can have high sensitivity and specificity, there can be positivity that is dependent on the antigen composition of the strains circulating in different geographic regions. In accordance with that consensus, serologic tests have limited clinical usefulness and their routine performance is not recommended.6
On the other hand, 31% of the physicians stated that they carried out more than one diagnostic test (usually 2) to diagnose H. pylori infection, and the most common combination was serology + histology. Albeit a minority, some physicians required 3 tests to make the diagnosis. Those results are striking, in that they reveal the lack of knowledge of the true clinical usefulness of the diagnostic tests or a lack of confidence as to their accuracy. Obviously, those practices result in great expense and are not very beneficial, significantly increasing costs in a country such as Mexico.
The therapeutic indications for H. pylori eradication are clearly specified in the Mexican Consensus on Helicobacter pylori. Among the main indications are: gastric or duodenal peptic ulcer, atrophic gastritis and intestinal metaplasia, type B gastric lymphoma (MALT) of the marginal zone, a history of gastric cancer, and the chronic use of NSAIDs in patients with associated risk factors.7 The same as in other studies involving primary care physicians, it was shown that the role of H. pylori eradication in patients with MALT gastric lymphoma was not known, and that eradication treatment was started without the support of an adequate diagnostic tool.
In Mexico, as in other parts of the world, first-line treatment continues to be the combination of a PPI plus amoxicillin and clarithromycin.15 Even though 65% of the general practitioners used this regimen, it was surprising that the rest of the regimens were varied, or even included regimens with no recommendations or support. It was also striking that the second most widely used treatment was quadruple therapy that included metronidazole. As we know, resistance to that antibiotic is as high as 53%, which has limited its use in Mexico for many years.16,17 And even though the percentage was very low, it was striking that regimens that have no scientific support were used, such as amoxicillin plus clavulanic acid or trimethoprim/sulfamethoxazole.
With respect to treatment duration, even though the majority of participants (75%) used eradication regimens for 14 days, 13% used regimens for more than 21 days and up to one month. Once again, not only is there a lack of evidence to support such prolonged schemes, but this type of recommendation can also be very costly, not well-tolerated (due to the side effects of the antibiotics), and promote the development of greater antimicrobial resistance.
The confirmation of eradication treatment is justified, for which there are noninvasive, easy-access methods, but the definitive choice of method depends on clinical context. Ahmed et al.13 reported that the most frequently used method was the serology test (47%), followed by the urea breath test (35%). However, the primary care physicians surveyed considered endoscopy the first choice for carrying out histologic study (33%), ignoring the noninvasive techniques that imply less risk and lower cost. Endoscopy obviously involves high cost and its use in this context is not very practical, nor is there any scientific evidence to support it. In addition, the fact that close to 15% of the general physicians surveyed stated they required more than 3 tests to corroborate eradication, underlines their lack of confidence in the diagnostic tests.
Our study, despite its interesting results, had the limitation of being a survey that was cross-sectionally applied to a group of general physicians during an academic event, and thus the information obtained could have collection bias, selection bias, nonresponse bias, or the volunteer effect. In addition, the questionnaire was not validated for content, construct, criterion, or reliability. Even so, we believe that the data obtained realistically reflects the knowledge about H. pylori in our environment.
In conclusion, our results showed there is a lack of knowledge about the diagnostic and treatment recommendations established for H. pylori infection. Therefore, we consider this a point of special interest in relation to continuing medical education. The implementation of workshops, courses, and conferences, or the formulation of practical guidelines, should be directed at primary care physicians to strengthen medical practice based on scientific evidence.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestDr. José María Remes-Troche is a Member of the Advisory Board of Takeda Pharmaceuticals, Alfa-Wassermann, and Almirall. He is a Speaker for Takeda, Asofarma, Alfa-Wassermann, Almirall, and Astra-Zeneca.
Please cite this article as: Cano-Contreras AD, Rascón O, Amieva-Balmori M, Ríos-Gálvez S, Maza YJ, Meixueiro-Daza A, et al. El abordaje, las actitudes y el conocimiento acerca de Helicobacter pylori en médicos generales es deficiente ¡Hay mucho que mejorar! Revista de Gastroenterología de México. 2018;83:16–24.