We present herein the case of a 30-year-old man with an unremarkable past medical history who sought medical attention for a tumor at the level of the left sternoclavicular joint, having had no previous trauma. Upon physical examination, a well-demarcated, fixed tumor adhered to the deep planes was palpated.
Soft tissue ultrasound showed a hypoechoic, heterogeneous mass with calcifications, marked vascularization, and a pattern of bone destruction in the adjacent clavicle.
The study of the patient was completed with MR imaging, which described a rounded mass in the proximal epiphysis of the left clavicle that was hypointense in T1 and mildly hyperintense in T2, presenting signs of aggressive behavior with cortical disruption (fig. 1).
The mass was biopsied, identifying an infiltrate due to tumor proliferation, with growth in nests of large cells with abundant granular eosinophilic cytoplasm. Immunohistochemistry showed cytoplasmic positivity for hepatocyte paraffin 1 (Hep Par-1), glypican-3 (GPC3), epithelial membrane antigen (EMA), and cytokeratin 7 (CK7). All results were consistent with metastasis due to hepatocellular carcinoma (HCC).
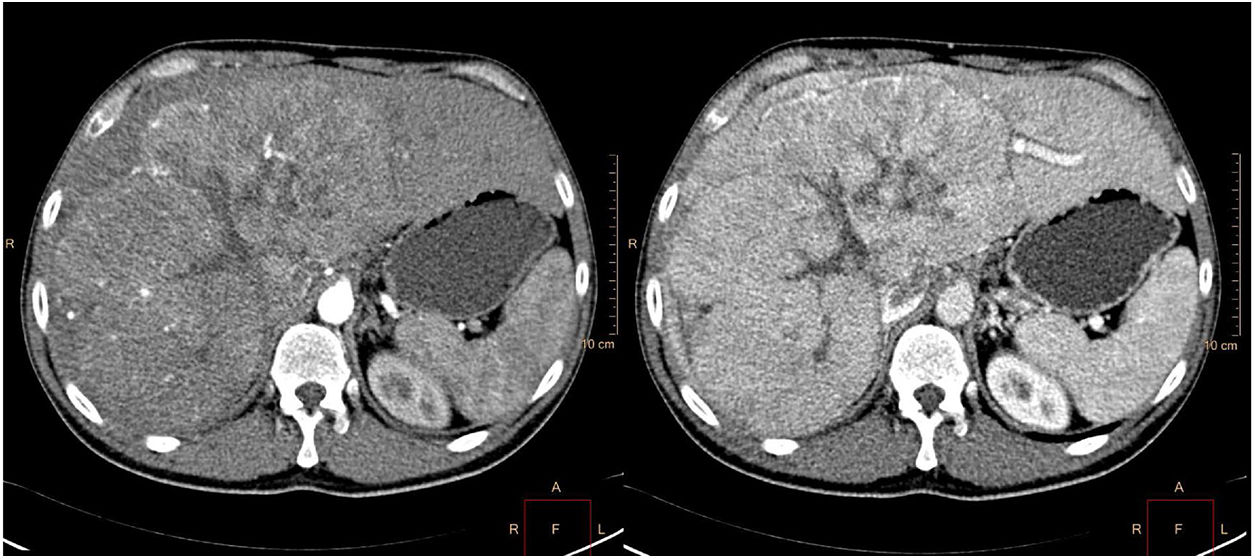
The patient was referred for consultation to complete his evaluation. Physical examination revealed hepatomegaly of the right hepatic lobe. Laboratory test results were: bilirubin 1.5mg/dl, AST 154 U/l, ALT 159 U/l, and alpha-fetoprotein 170119 ng/ml (0-6). An abdominal CAT scan was ordered and identified a mass on the right hepatic lobe measuring 23cm in diameter, with a central stellate scar and lobulated contours, as well as very patent vascularization in the arterial phase, heterogeneous enhancement in the portal phase, and wash-out in the equilibrium phase (fig. 2).
Axial reconstruction in a multi-slice CAT scan in the arterial (a) and portal (b) phases after contrast-medium administration: a mass measuring 23cm in diameter in the right hepatic lobe, with patent vascularization in the arterial phase and heterogeneous enhancement in the portal phase.
Given the clinical context and immunohistochemical profile, stage IV fibrolamellar hepatocellular carcinoma (FLHCC) was diagnosed. Chemotherapy was begun with gemcitabine and oxaliplatin (GEMOX) and palliative radiotherapy on the clavicular lesion, with follow-up by the Oncology Service.
FLHCC is a rare variant of HCC and accounts for 1-9% of all primary hepatocellular carcinomas, with a yearly incidence of 0.02 cases/100,000 inhabitants.1 It mainly affects persons under 40 years of age, with no difference between the sexes, and the majority of cases are in patients with no prior hepatopathy.2
It is caused by the DNAJB1-PRKACA mutation on chromosome 19, with 8 genes included in the deletion, the most common of which are MUC4 (associated with other gastrointestinal tumors) and GOLCA6L2.3
Symptoms are usually nonspecific (abdominal pain, bloating, jaundice), resulting in 70% of cases diagnosed at advanced stages of the disease. Other unusual presentations of FLHCC have been reported, such as Budd-Chiari syndrome, hemoperitoneum, gynecomastia, bone metastasis, acute liver failure, and the paraneoplastic syndromes of hypoglycemia, hyperthyroidism, and deep vein thrombosis.4
The most frequent dissemination route in FLHCC is via the lymph nodes (50-70%), and venous or arterial invasion is rare. The most frequent distant metastasis sites are the lung, peritoneum, and adrenal glands.5 Alpha-fetoprotein is elevated in a minority of cases.6
Radiology is essential for diagnosis, requiring multi-phasic studies through CT and/or MR imaging for an accurate evaluation. The differential diagnosis should be made with other focal hepatic lesions, such as focal nodular hyperplasia, hepatocellular adenoma, classic HCC, and liver metastases.
CT study tends to identify a large, well-defined, polylobulated, heterogeneous lesion that is hypodense with no contrast medium and with calcifications (40-68%). Around 70% have a non-pathognomonic central stellate scar. There is early heterogeneous enhancement in the arterial phase and enhancement varies in the portal and equilibrium phases.7
In MR imaging, FLHCC is hypointense in the T1-weighted sequences and hyperintense in the T2-weighted sequences, whereas the central scar is hypointense in the two sequences.
Nevertheless, the majority of radiologic findings are not conclusive for diagnosis and histologic studies are required. Regarding the immunohistochemical profile, positive staining for Hep Par-1 and GPC3 is similar to that in HCC, but CK7, EMA, and CD68 are only positive in FLHCC.8
Liver resection and liver transplantation are the only potentially curative treatment options. Aggressive liver resection is the treatment of choice in the majority of cases. Its 5-year survival rate varies from 26-76%9 and the 5-year disease-free survival is low (18%). However, even in patients with advanced disease, aggressive surgery appears to be beneficial in terms of survival.10 Currently, the role of chemotherapy in FLHCC is controversial, given the lack of quality studies that demonstrate a survival benefit.
FLHCC has traditionally been considered less aggressive than classic HCC, but that is now being questioned because at a similar stage and in non-cirrhotic patients, FLHCC does not have a better prognosis than HCC, nor does it respond differently to treatment. Therefore, it has been suggested that both the absence of cirrhosis and young age at diagnosis are possible reasons for considering potentially curative treatments in a greater number of patients with FLHCC.11
In conclusion, the diagnosis of FLHCC requires the combination of clinical, radiologic, and histologic findings. The peculiarity of the case presented herein was the unusual presentation in the form of a metastatic clavicle tumor. That metastatic site has been described in the literature in relation to other tumors (papillary thyroid cancer,12 pheochromocytoma) but there are no published cases of clavicle tumor secondary to FLHCC.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Cebrián A, Elosua A, González-de la Higuera B, Irisarri R, Ruiz-Clavijo D. Tumoración clavicular como manifestación inicial de un hepatocarcinoma fibrolamelar. Revista de Gastroenterología de México. 2020;85:104–106.