Although some studies suggest that the prevalence of cholelithiasis (from 22 to 30%) is greater in patients that are in substitutive renal therapy, whether it be hemodialysis (HD)1 or peritoneal dialysis (PD),2 when compared with the healthy population, other studies report that this prevalence is similar (3.8% in patients with renal failure and 1.5% in healthy subjects). In Mexico, the raw prevalence of cholelithiasis is less than 20%3 and there are no studies on the prevalence of biliary stones in patients with renal failure. The clinical manifestations of these patients may vary from abdominal pain and peritonitis to the dramatic clinical symptoms of perforated cholecystitis with frankly purulent dialyzing fluid.
Patients presenting with chronic renal failure (CRF) that required HD or PD usually are immunosuppressed and have different grades of coagulopathy,4 which increases the risk for bleeding and infection. In addition, these patients present with other intrinsic risks such as adherences due to peritonitis, peritoneal thickening secondary to PD, violation of the peritoneum in open abdominal procedures, and the temporary suspension of dialysis.
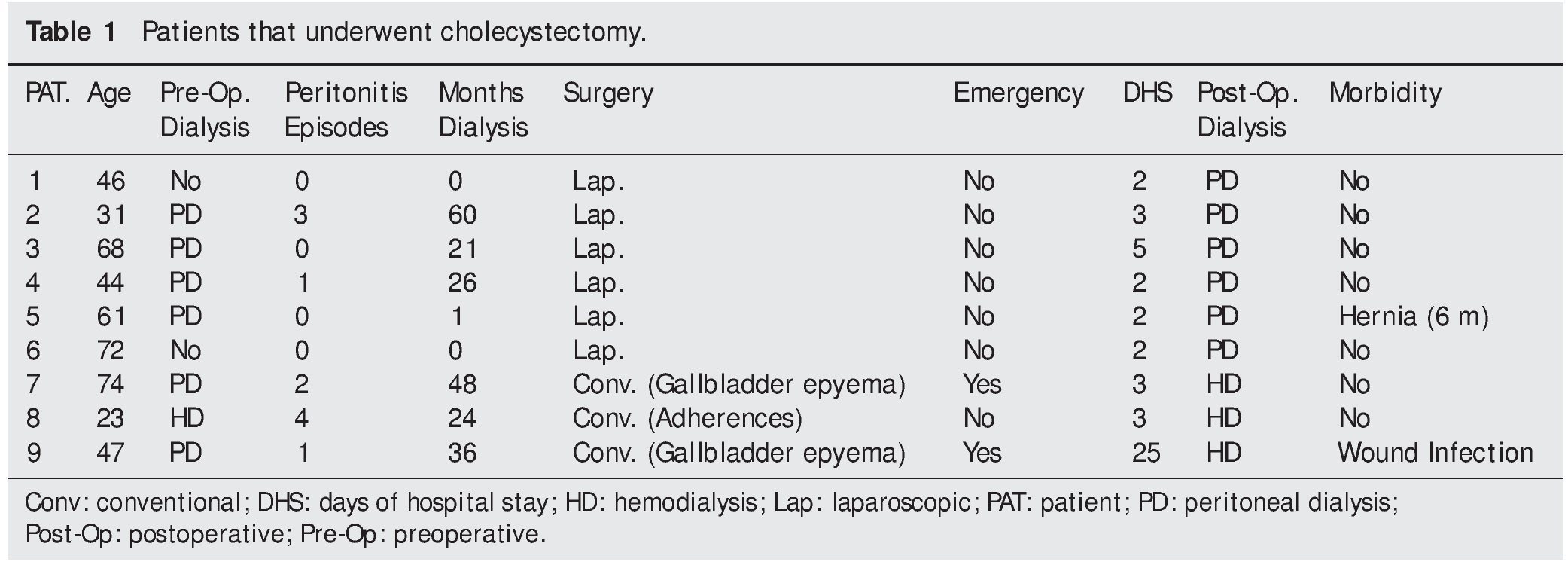
The aim of this study communication was to retrospectively review the results of CRF patients in HD or PD that underwent cholecystectomy due to cholelithiasis in 2 tertiary care hospitals in the city of Veracruz. Within the time frame of January 2005 to December 2008, 9 patients underwent cholecystectomy due to symptomatic cholelithiasis (repeated symptoms of pain in the right hypochondrium, liver function test alterations and/or ultrasound evidence of acute cholecystitis). Two patients underwent emergency surgery (Table 1).
Seven of the 9 patients were men and the mean age of all the patients was 51.8 ± 18.1 (23-74) years. The mean weight was 71.4 ± 11.4 (51-90) kg and the mean body mass index was 26.4 ± 3.3 (22-36). Diabetes mellitus was the cause of renal failure in 55.5% of the cases (n=5). The mean preoperative hemoglobin was 9.64 ± 1.36 (7.3-11.5) g/dL. The mean blood ureic nitrogen and serum creatinine were 61 ± 23 (33-97) mg/ dL and 8.3 ± 4 (3.4-14.9) mg/dL, respectively; serum albumin was 3.14 ± 0.76 (1.8-4.1) g/dL. Table 1 shows the results that were pertinent to the method of dialysis, the type of surgery, and the postoperative progression. Pneumoperitoneum creation through the open technique was performed in all of the patients that underwent laparoscopic cholecystectomy. Two patients had an additional surgical procedure to the cholecystectomy (patient 2: umbilical hernia and patient 6: right inguinal hernia repair). Morbidity was present in 2 cases; one post-incisional hernia, the same as occurred in a patient that underwent elective surgery (1/6, 16%), and surgical wound infection in one of the patients that had urgent surgery (1/2, 50%). There was no mortality and progression was favorable in all the cases.
The present case series lends support to the evidence that, when dealing with CRF patients with cholelithiasis, surgical treatment through cholecystectomy, preferably laparoscopic, is a safe and effective procedure with low morbidity. There are very few studies in the medical literature on CRF patients that underwent cholecystectomy. The majority of them report on isolated cases that discuss the feasibility of laparoscopic cholecystectomy in patients with PD.5-8 In addition to the well known advantages of laparoscopic cholecystectomy in the population in general, the avoidance of peritoneal violation in open procedures and the consequent prevention of dialyzing fluid leakage, the use of the PD catheter as a noninvasive method of pneumoperitoneum,5,6 and the early re-establishment of PD are all additional benefits of laparoscopic cholecystectomy in CRF patients. In some cases laparoscopic cholecystectomy can be combined with other procedures, such as abdominal wall correction,8 without affecting morbidity, as was carried out in one of our patients.
As part of the postoperative progression of the patient in PD that has undergone cholecystectomy, early re-initiation of dialysis, whether intermittent or low-volume, should be considered. Holley, et al.9 proposed a regimen of intermittent PD for 3 days followed by low volume PD. Our team has a regimen of postoperative low volume PD, previously described, that is begun in the first 48 hours after surgery.10 Even though some authors consider that PD patients should have a period of HD after laparoscopic cholecystectomy,5 only 2 of our patients changed the dialysis method after surgery, and they were patients that had undergone conventional cholecystectomy; these findings were similar to those of Nelson et al.2
Despite the small size of our case series, it showed a similar morbidity to that reported in other case series. And finally, even though it was not the aim of our case series, it should be explained that we did not have a true prevalence of cholelithiasis in our CRF population with or without some type of renal substitution therapy. Knowing this prevalence could lead us to the true incidence of cholecystitis in this type of patient in order to develop a surveillance strategy for this pathology and reduce its morbidity even more.
Financial disclosure
No financial support was received in relation to this article.
Conflict of interests
Dr. José María Remes-Troche is a Member of the Advisory Board of Takeda Pharmaceuticals, Alfa-Wasserman, and Janssen and a Speaker for Nycomed-Takeda, Advance Medical, Astra-Zeneca, and Bristol-Myers-Squibb. He receives research support from Sanofi¿Pasteur.
*Corresponding author at:
Corporativo San Gabriel. Alacio Pérez 3er. Piso. Col. Veracruz Ver. Mexico. 91700.
Tel.: +(229) 932-7782; fax: +(229) 932-7782.
Email address:gmtzmier@hotmail.com (G. Martínez-Mier).