Capsule endoscopy has revolutionized the study of small bowel disorders. Its diagnostic yield, reasons for referral, and frequency of significant endoscopic findings at our institution are unknown. The aims of our study were to describe the reasons for referral, the frequency of significant endoscopic findings, and the diagnostic yield of capsule endoscopy in patients that underwent the procedure for the study of small bowel disorders.
Materials and methodsA retrospective study was conducted that included all patients that underwent capsule endoscopy for small bowel disorder evaluation at our institution. The diagnostic yield for significant endoscopic findings, the frequency of significant endoscopic findings, and the reasons for referral for capsule endoscopy were determined.
ResultsA total of 134 patients were included in the study and 143 capsule endoscopies were performed. Women made up 48.5% of the sample and the mean patient age was 63 years (18.7 standard deviation). The main reasons for referral were suspicion of overt small bowel bleeding (55.9%) and suspicion of occult small bowel bleeding (28.6%). The overall diagnostic yield was 66.4%. The most common significant findings were small bowel angioectasias (52.6%) and small bowel ulcers (38.9%). There were two adverse events (1.3%): one capsule retention that required enteroscopic removal and one asymptomatic bronchoaspiration of the capsule that resolved spontaneously.
ConclusionsThe frequency of significant endoscopic findings with capsule endoscopy at our institution was different from that reported in other Mexican studies, but the reasons for referral and the diagnostic yield were similar.
La cápsula endoscópica ha revolucionado el estudio de patologías del intestino delgado. Desconocemos su rendimiento diagnóstico, motivo de referencia y la frecuencia de hallazgos endoscópicos significativos en nuestra institución. Los objetivos del studio fueron: describir los motivos de referencia, la frecuencia de hallazgos endoscópicos significativos y el rendimiento diagnóstico de la cápsula endoscópica en pacientes sometidos a esta para estudio de patologías de intestino delgado.
Material y métodosSe llevó a cabo un estudio retrospectivo en el cual se incluyeron todos los pacientes a los que se les realizó una cápsula endoscópica para estudio de patología en intestino delgado en nuestra institución. Se determinó el rendimiento diagnóstico para hallazgos endoscópicos significativos, la frecuencia de hallazgos endoscópicos significativos y la frecuencia de los motivos de referencia para cápsula endoscópica.
ResultadosSe incluyeron 134 pacientes a los cuales se les realizaron 143 cápsula endoscópica; el 48.5% fueron mujeres, con una edad promedio de 63 años (desviación estándar 18.7). Los principales motivos de referencia fueron sospecha de hemorragia de intestino delgado manifiesta (55.9%) y sospecha de hemorragia de intestino delgado oculta (28.6%). El rendimiento diagnóstico global fue del 66.4%. Los principales hallazgos significativos fueron angioectasias en intestino delgado (52.6%) y úlceras en intestino delgado (38.9%). Hubo 2 eventos adversos (1.3%): una retención de cápsula endoscópica que requirió recuperación por enteroscopia y una broncoaspiración asintomática de cápsula endoscópica que resolvió espontáneamente.
ConclusionesLa frecuencia de hallazgos endoscópicos significativos con cápsula endoscópica difiere en comparación con otros estudios en México; sin embargo, los motivos de referencia, así como el rendimiento diagnóstico de esta en nuestra institución, son similares.
Gastrointestinal endoscopy has advanced impressively over the past decades. The evaluation of small bowel (SB) disorders had always been a challenge until the advent of new technologies, such as capsule endoscopy (CE) of the SB and deep enteroscopy. Since its appearance in Western countries in 2001, CE has revolutionized the study of the SB, thanks to its mildly invasive, reliable technique for viewing that portion of the intestine, which could not be achieved through conventional endoscopy.
The main disorders in which it has played an important role are: small bowel bleeding (SBB), iron deficiency anemia, Crohn’s disease (CD), celiac disease, SB tumors, and hereditary polyposis syndromes. Its usefulness in those pathologies is described in numerous international guidelines.1–5
The term gastrointestinal bleeding of obscure origin (GIBOO), previously defined as that in which the cause of bleeding was not identified with conventional endoscopy (upper endoscopy and colonoscopy), has been modified, thanks to CE and deep enteroscopy. Today it is defined as bleeding whose origin is not identified, despite a complete gastrointestinal tract evaluation that includes the SB. What was previously known as GIBOO is now referred to as suspected SBB. It can be overt or occult, if it presents or not with clinical signs of bleeding, such as hematemesis, coffee ground vomitus, hematochezia, melena, or rectorrhagia.2,4
The traditional parameters of diagnostic accuracy are difficult to determine in those pathologies, given that there is no gold standard. Thus, the parameter that is used for the study of diagnostic accuracy is diagnostic yield (DY), which is defined as the detection rate of a clinically significant finding. The overall DY of CE is around 60%6–10 and varies depending on the reason for referral (92.3% vs. 44.2% in suspected overt SBB vs. suspected occult SBB).11
CE has been available at our healthcare institution since 2012, but its usefulness for SB disorders in our environment has not been studied.
The aims of our study were to describe the reasons for referral for CE of the SB, to determine the DY of CE for significant endoscopic findings in patients with a suspected SB disorder, and the frequency of significant endoscopic findings in those patients.
Materials and methodsA retrospective, descriptive study was conducted that included patients referred for CE due to the suspicion of a SB disorder, within the time frame of April 2012 to May 2018. The inclusion criterion was that the patients were referred for CE due to a suspected SB disorder. The exclusion criterion was not having a complete report of the endoscopic study.
For bowel preparation, one day before the study, patients began a liquid diet after their afternoon meal. At night, they received 2 liters of oral polyethylene glycol (PEG). The video capsule was administered orally by a nurse on the following day, after the patient had fasted for 10h. If the capsule required endoscopic administration, the patient was sedated by an anesthesiologist and the capsule was deposited into the duodenum, using a gastroscope and a net. If the patient had undergone bowel preparation for a colonoscopy, the capsule was administered orally after recovery from the colonoscopy or endoscopically during the sedation of the colonoscopic procedure, depending on the criterion of the endoscopist.
Once the capsule was administered, clear liquids could be taken after 2h, and a bland diet after 4h. The patient returned the next day for removal of the external data recorder, and if the patient was hospitalized, it was removed by a nurse.
The video capsules utilized in the present study were the MiroCam 1000-W, PillCam SB, SB2, and SB3 models. The studies were reviewed and interpreted by 2 different endoscopists trained in CE interpretation. If the video capsule did not reach the colon during the study and the patient was not aware of having expelled the capsule by day 15, an abdominal x-ray was taken to rule out capsule retention.
The variables analyzed were: age, sex, video capsule model, reason for referral, administration route, gastric transit time, intestinal transit time, study completion, significant endoscopic findings, and adverse events.
For the statistical analysis, proportions were employed for the qualitative variables. Mean and standard deviation (SD) were used for the parametric quantitative variables, and median and interquartile range (IQR) for the non-parametric variables. DY was calculated as the number of studies with significant endoscopic findings divided by the total number of studies performed.
Ethical considerations: All the patients signed statements of informed consent for CE performance. The study was authorized by the institution’s research ethics committee. The authors declare that this article contains no personal information that could identify the patients.
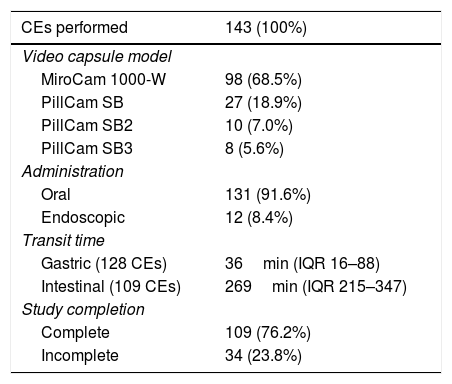
ResultsDuring the study period, 138 patients were referred for CE to evaluate SB disorders. Four patients were excluded because their endoscopic reports were incomplete. A total of 134 patients were included in the analysis, of whom 65 (48.5%) were women and 69 (51.5%) were men. Mean patient age was 68.5 years (IQR 53–77 years), with a range of 16–95 years. A total of 143 CEs were performed, given that 7 patients underwent a repeat CE and one patient had 2 repeat procedures. Ninety-eight CEs (68.5%) were carried out using the MiroCam 1000-W video capsule, 27 (18.9%) with the PillCam SB capsule, 10 (7.0%) with the PillCam SB2 capsule, and 8 (5.6%) with the PillCam SB3 capsule (Table 1). A total of 131 video capsules were administered orally (91.6%) and 12 were administered endoscopically (8.4%). Thirty-four studies were incomplete (23.8%). Of the 131 orally administered capsules, 3 (2.3%) did not pass into the duodenum (2 because of retention in the stomach and one due to asymptomatic capsule aspiration). Of the 12 capsules administered endoscopically, 2 did not reach the cecum (16.7%). Median gastric transit time of the orally administered video capsules that passed into the duodenum was 36min (IQR 16–88min), with a range of 1–627min. Of the 109 completed studies, the median intestinal transit time was 269min (IQR 215−347min), with a range of 83–695min.
CEs performed, models utilized, administration route, transit time, and study completion.
| CEs performed | 143 (100%) |
|---|---|
| Video capsule model | |
| MiroCam 1000-W | 98 (68.5%) |
| PillCam SB | 27 (18.9%) |
| PillCam SB2 | 10 (7.0%) |
| PillCam SB3 | 8 (5.6%) |
| Administration | |
| Oral | 131 (91.6%) |
| Endoscopic | 12 (8.4%) |
| Transit time | |
| Gastric (128 CEs) | 36min (IQR 16–88) |
| Intestinal (109 CEs) | 269min (IQR 215–347) |
| Study completion | |
| Complete | 109 (76.2%) |
| Incomplete | 34 (23.8%) |
CE: capsule endoscopy; IQR: interquartile range.
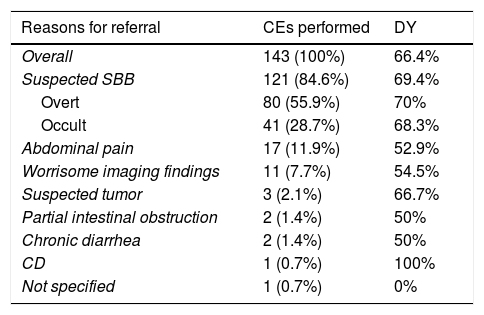
The reasons for referral were: suspected overt SBB in 80 patients (55.9%) and suspected occult SBB in 41 (28.7%), abdominal pain in 17 (11.9%), worrisome SB imaging findings in 11 (7.7%), suspected SB tumor in 3 (2.1%), recurrent partial intestinal obstruction in 2 (1.4%), chronic diarrhea in 2 (1.4%), CD in one (0.7%), and not specified in one (0.7%). Importantly, some of the patients had numerous reasons for CE referral (Table 2).
Reasons for referral and DY.
| Reasons for referral | CEs performed | DY |
|---|---|---|
| Overall | 143 (100%) | 66.4% |
| Suspected SBB | 121 (84.6%) | 69.4% |
| Overt | 80 (55.9%) | 70% |
| Occult | 41 (28.7%) | 68.3% |
| Abdominal pain | 17 (11.9%) | 52.9% |
| Worrisome imaging findings | 11 (7.7%) | 54.5% |
| Suspected tumor | 3 (2.1%) | 66.7% |
| Partial intestinal obstruction | 2 (1.4%) | 50% |
| Chronic diarrhea | 2 (1.4%) | 50% |
| CD | 1 (0.7%) | 100% |
| Not specified | 1 (0.7%) | 0% |
CE: capsule endoscopy; CD: Crohn’s disease; DY: diagnostic yield; SBB: small bowel bleeding.
Overall DY for CE was 66.4%. There was a relevant upper or lower gastrointestinal finding in 6.9%. Particularly in suspected SBB, DY was 69.4%; 70% when the SBB was overt and 68.3% when it was occult. The DY for other reasons for referral was: abdominal pain (52.9%), worrisome SB imaging studies (54.5%), suspected SB tumor (66.7%), recurrent partial intestinal obstruction (50%), chronic diarrhea (50%), CD (100%), and non-specified reason (0%).
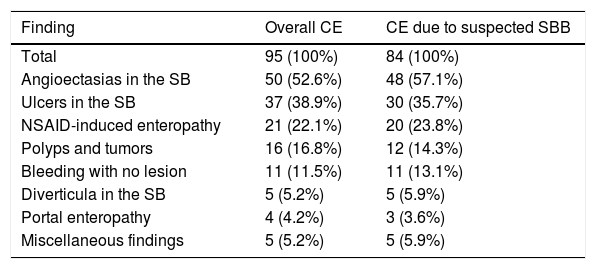
There were significant endoscopic findings in 95 CEs: SB angioectasias in 50 (52.6%), SB ulcers in 37 (38.9%), enteropathy due to nonsteroidal anti-inflammatory drug (NSAID) use in 21 (22.1%), SB polyps or tumors in 16 (16.8%), bleeding with no apparent lesion in 11 (11.5%), SB diverticula in 5 (5.2%), portal enteropathy in 4 (4.2%), and miscellaneous findings in 5 (5.2%). Particularly in suspected SBB, the main significant finding was SB angioectasias in 48 CEs (57.1%), SB ulcers in 30 (35.7%), NSAID-induced enteropathy in 20 (23.8%), SB polyps or tumors in 12 (14.3%), bleeding with no apparent lesion in 11 (13.1%), SB diverticula in 5 (5.9%), portal enteropathy in 3 (3.6%), and miscellaneous findings in 5 (5.9%). The miscellaneous causes were actinic enteritis, angioectasias in the colon, nonspecific mucosal inflammation, gastric angioectasias, and congestive enteropathy in a patient with heart failure. Some CEs had numerous different findings (Table 3).
Significant endoscopic findings.
| Finding | Overall CE | CE due to suspected SBB |
|---|---|---|
| Total | 95 (100%) | 84 (100%) |
| Angioectasias in the SB | 50 (52.6%) | 48 (57.1%) |
| Ulcers in the SB | 37 (38.9%) | 30 (35.7%) |
| NSAID-induced enteropathy | 21 (22.1%) | 20 (23.8%) |
| Polyps and tumors | 16 (16.8%) | 12 (14.3%) |
| Bleeding with no lesion | 11 (11.5%) | 11 (13.1%) |
| Diverticula in the SB | 5 (5.2%) | 5 (5.9%) |
| Portal enteropathy | 4 (4.2%) | 3 (3.6%) |
| Miscellaneous findings | 5 (5.2%) | 5 (5.9%) |
CE: capsule endoscopy; NSAID: nonsteroidal anti-inflammatory drug; SB: small bowel; SBB: small bowel bleeding.
There were 2 adverse events (1.4%): one capsule retention in the SB that required retrograde enteroscopy for its resolution and one asymptomatic 10h capsule aspiration that was spontaneously expectorated by the patient. With respect to technical problems, one video capsule (0.7%) stopped transmitting after 16min.
Discussion and conclusionsSince its appearance in the West in 2001, numerous studies have evaluated the diagnostic capacity of CE. Such analyses have been published since 2005 in Mexico.12–19 The present study is one of the largest Mexican case series, with a total of 143 CEs performed.
The principal usefulness of CE has been demonstrated in SBB, which is its main indication. It has been shown to be less useful in other indications, such as CD, celiac disease, and SB tumors. In our study, the primary reason for referral was suspected SBB (84.6%), similar to that reported in other studies conducted in Mexico. In a study by Teramoto-Matsubara et al.,12 in which 42 CEs were performed, the main indication was GIBOO in 24 cases and anemia in 6. Santoyo-Valenzuela et al.15 described similar findings in 45 cases, with 71.11% of the CEs referred for GIBOO. In a study on 60 patients by Hernández-López et al.,17 40 CE referrals were due to GIBOO. Cuba-Sascó et al.18 conducted a comparative study with CE, in which the main reason for referral was GIBOO in 19 out of 29 patients (63.3%). In our study, abdominal pain was the reason for referral in 17 CEs, 12 of which had an additional reason for referral, such as suspected SBB, worrisome SB imaging studies, or suspected SB tumor. It should be mentioned that abdominal pain is not a duly established indication for CE in the literature. Two CEs were also performed in patients with a history of partial intestinal obstruction. Special care must be taken in those types of patient before performing CE. Due to the risk for capsule retention, previous computed tomography or magnetic resonance imaging is recommended.2 In patients at high risk for capsule retention, the administration of a dissolvable capsule to assess luminal patency, which has good accuracy for predicting the possibility of endoscopic video capsule retention, is advisable. Abdominal pain, bloating, nausea, vomiting, intestinal resection, abdominal or pelvic radiotherapy, chronic high-dose NSAID use, and the suspicion or presence of inflammatory bowel disease, are established risk factors for capsule retention. At our institution, we did not have access to the capsule permeability test at the time of the present study. The 2 patients whose reasons for CE referral were partial intestinal obstruction had addition reasons: one patient had an imaging finding of inflammation and thickening of the ileum and the other patient had suspected occult SBB. Both had imaging studies prior to CE, and they did not present with adverse events.3
Our results showed an overall DY of 66.4%; 69.4% for suspected SBB, in which it was slightly higher in overt SBB versus occult SBB (70% vs. 68.3%). DY was lower for the other reasons for referral, most likely related to fewer CEs performed for those indications and the lower usefulness of CE in those pathologies. In several meta-analyses, the DY of CE for SBB was around 60%.6–11 DY improves considerably in overt bleeding if it is active or if the procedure is performed early.11,20–22 The DY for CD is 52%,23 there are many false negatives for tumors,24,25 and DY for celiac disease is still controversial.26 In Mexico, the DY of CE for SBB varies from 65% to 82%.12–14,16,17 We believe our DY could be lower than that reported in other Mexican studies because of our larger sample size, as demonstrated in the abovementioned meta-analyses that have a larger number of patients. The slight difference we found between overt SBB and occult SBB was probably due to the fact that the CEs were performed late in the patients with suspected overt SBB. However, we did not have all the necessary clinical data of those patients to carry out that analysis.
The main significant endoscopic findings were SB angioectasias in overall CE performance and in those carried out due to suspected SBB (52.6% and 57.1%), followed by SB ulcers. Indeed, angioectasias are the most widely described lesions, reported at 20–30% in cases of SBB.9,27,28 In Mexico, Teramoto-Matsubara et al.12 identified angioectasias in 11 patients (61.1%), followed by ulcers in 4 (22.2%). García-Compean et al.13 found angioectasias in 36%, ulcers in 25%, and neoplasias in 21%. In another study conducted by Hernández-López et al.,17 angioectasias were the main finding in 36%, followed by NSAID-induced ulcers in 21%. Nevertheless, numerous Mexican studies describe contrasting results. Santoyo-Valenzuela et al.15 reported erosions in 22% as the primary finding, followed by vascular alterations in 17.7%, and polyps in 13.3%. In a study on 49 patients, Blanco-Velasco et al.16 found ulcers in 16 (32.6%), angioectasias in 10 (20.4%), and ulcerated tumors in 2 (4.1%). In a study by Cuba-Sascó et al.,18 the main finding was ulcer in 31% of the patients, followed by angioectasias in 13.8%, stricture in 13.8%, and submucosal tumor in 10.3%. We believe that angioectasias are very frequent findings in those cases, but it is difficult to know if they are the cause of the bleeding in all the cases observed, given that evaluations are often subjective and depend on the criterion of the endoscopist interpreting the CE.29
CE is a relatively safe study with a low risk for adverse events. Its main complications are capsule retention and capsule aspiration. In one of the largest studies, capsule retention occurred in 1.87% of the CEs and capsule aspiration in 0.003%.30 In our study, the adverse event rate was 1.4%, with one case of capsule retention and one of capsule aspiration. It is our opinion that as the number of CEs performed increases, the capsule retention rate could also increase, and the aspiration rate could decrease. It is important to detect the adverse event risk factors in patients, such as advanced age, neurologic disorders, or swallowing disorders, providing a window of opportunity in our service for deciding on the capsule administration route.
Among the limitations of the present study is its solely retrospective and descriptive design. Because many patients were referrals, the clinical information before and after CE was incomplete or unknown. Follow-up could not be carried out to determine the therapy employed or the final diagnosis of the findings. Because patients were referred from the private medical sector and our institution did not initially have an endoscopist that reviewed all the reasons for referral in the process of CE performance, its indication was unclear in some of the procedures. The significant endoscopic findings were reported subjectively, given that standardized classifications were not used in the reports. Despite those limitations, the present study is one of the largest case series on CE conducted in Mexico.
In conclusion, CE is a vastly important tool for studying SB disorders, especially SBB. The reasons for referral and the DY at our institution were similar to those reported in other studies conducted in Mexico, but the significant endoscopic findings were different.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this study.
Author contributionsD. Keil-Ríos contributed to the drafting of the manuscript and data acquisition. Angulo-D. Molina contributed to the concept of the study and its design. M. Peláez-Luna contributed to the data analysis and interpretation. A. Farca-Belsaguy and J. Estradas-Trujillo contributed to the critical review of the intellectual content.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Keil-Ríos D, Angulo-Molina D, Peláez-Luna M, Farca-Belsaguy A, Estradas-Trujillo J. Cápsula endoscópica para el estudio de patologías de intestino delgado: experiencia en una institución privada en México. Revista de Gastroenterología de México. 2020;85:240–245.